Dr Seth Berkley, Gavi the Vaccine Alliance
Early in my medical career, in the 1980s, I worked as a field epidemiologist in Uganda, evaluating immunisation programs and conducting research into HIV. This is what first set me on a course to spearhead the International AIDS Vaccine Initiative (IAVI), but it was also my first exposure to shockingly high levels of child mortality. The reason for this? At the time, vaccination coverage in Uganda was incredibly low, with almost three-quarters of kids not getting even basic vaccine protection. It was a similar story in many other poor countries.
More than 30 years later, I now have the privilege of being CEO of Gavi, the Vaccine Alliance. Today, basic global vaccination coverage is 86%, with coverage for the poorest countries, those supported by Gavi, coming in at 81%. But the lifesaving mission of immunisation is far from over. Here’s why vaccines still have an essential role to play in the future of global health:
1) Protecting the world’s most vulnerable people
Global vaccination coverage figures are looking up, but they still mask huge inequalities that we cannot afford to ignore. In 2015, more than 19 million children were still not fully protected by even the most basic routine immunisation. These children often come from the poorest, most marginalised families, and the hardest-to-reach communities.
2) We have more vaccines against the biggest killers
My father was given only one vaccine, smallpox. I received a handful. My children have been vaccinated against meningitis, pneumonia, diarrhoea, hepatitis B, and many of the biggest killers of children. However, full coverage with the 11 vaccines that the World Health Organization (WHO) recommends for all children is only about 5%. We need to get these universally introduced to keep children healthy and able to live up to their full potential.
3) The foundation of health systems
That said, no other health intervention reaches as many people globally as immunisation. This gives vaccines the edge when it comes to improving equitable access to healthcare – they can be the foundation for other, much needed health services. As vaccines don’t introduce themselves, reaching the most marginalised groups can open up pathways for other types of healthcare, and we’re already seeing how access to human papillomavirus (HPV) vaccinations to prevent cervical cancer can open a window of opportunity to provide other vital health services for previously unreached adolescent girls.

A girl receives the HPV vaccine. Laos, 2013. Photo by: Gavi / Bart Verweij
4) Part of the solution to antimicrobial resistance
Antimicrobial resistance – where pathogens develop resistance to previously effective drugs – could cause 10 million deaths per year by 2050. The severity of this issue has prompted the UN and world leaders to pledge to take urgent action. While behavioural change and development of new antibiotics are absolutely essential, vaccines also have an important role to play in ensuring that infections don’t occur in the first place.
5) The moonshots we already have against cancer
US Vice President Joe Biden’s call for a “cancer moonshot” was greeted with excitement earlier this year, and rightly so. But we shouldn’t forget that we already possess tools to fight the causes of certain cancers: HPV and hepatitis B vaccinations can help to prevent cervical and liver cancers, among others. As the burden of cancer grows, particularly in developing countries where access to screening and treatment is more limited, we need to make sure all children have access to these “moonshot” vaccines.
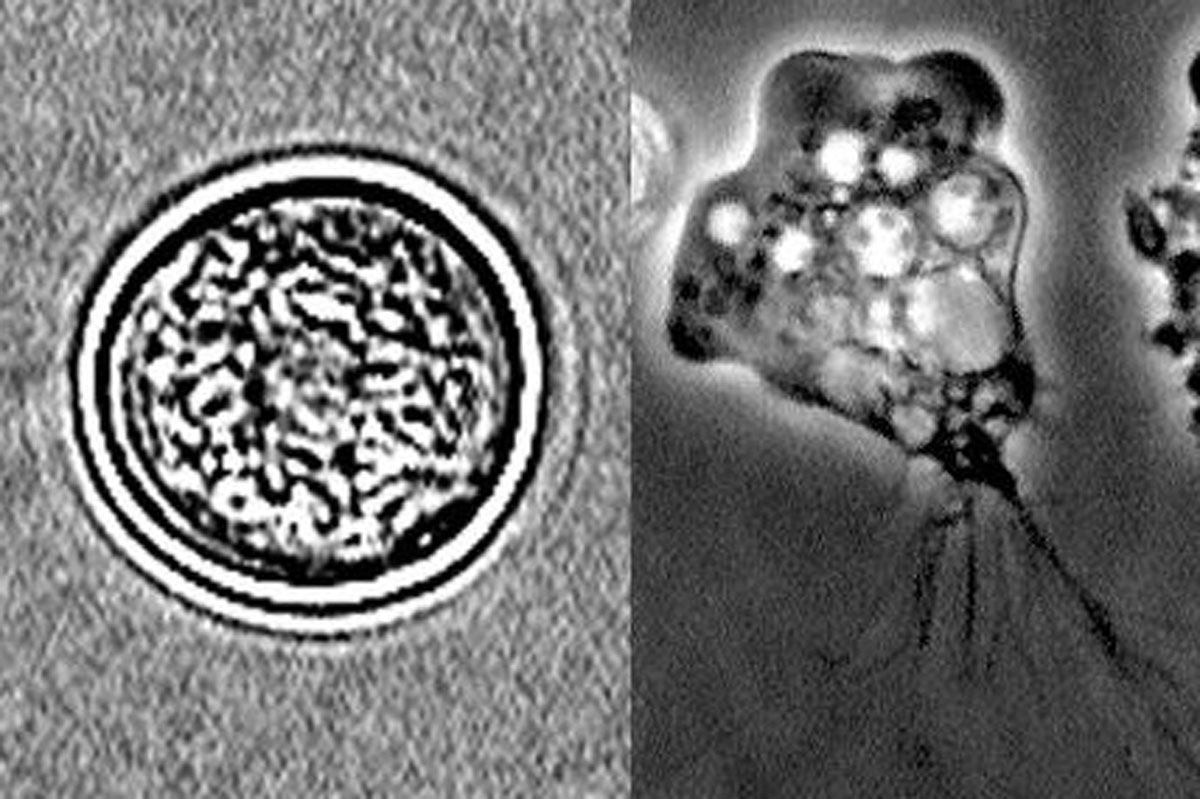
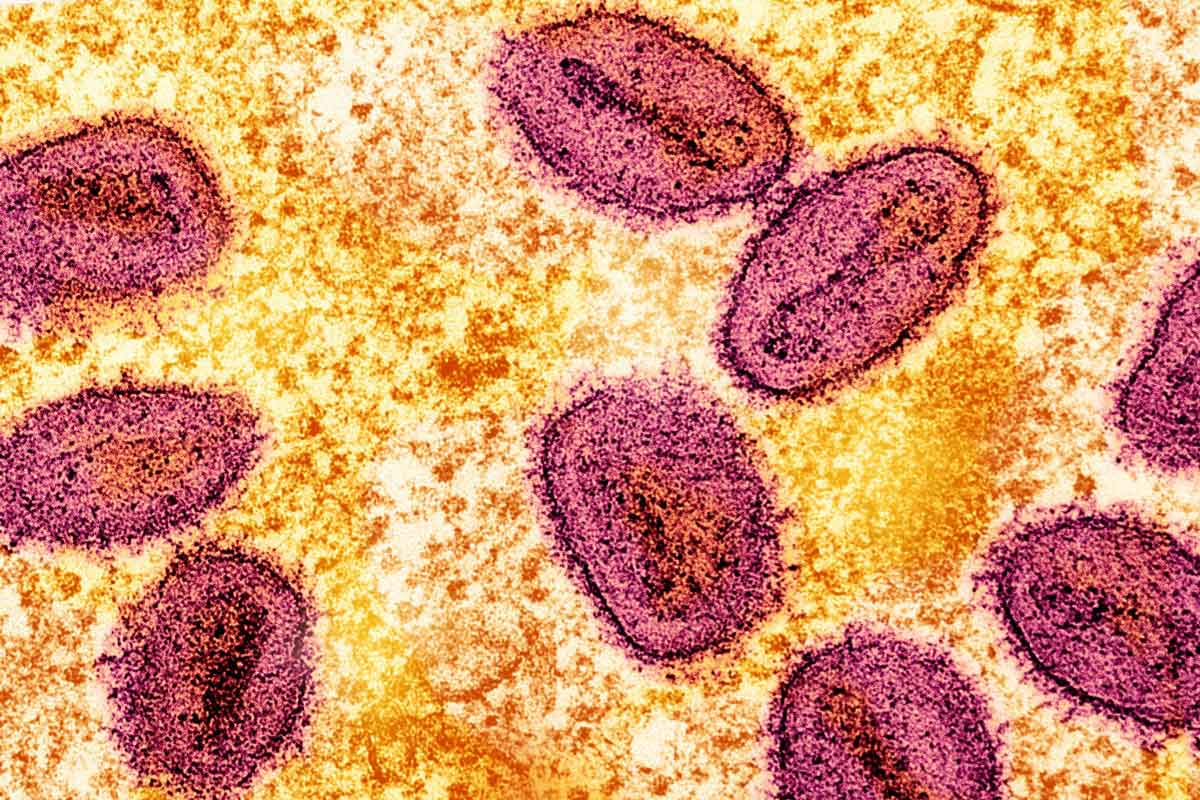
6) Tools to counter growing outbreak risks
Yellow fever, Ebola, Zika, bird flu – whatever epidemic is next, vaccines will be needed as part of the solution. As populations continue to grow, alongside climate change and urbanisation, it will be increasingly necessary to have high herd immunity for the diseases we know are waiting to strike. This means strong routine immunisation and adequate vaccine stockpiles, while also preparing for diseases we currently know less about. The Coalition for Epidemic Preparedness Innovations (CEPI) has been set up to lead the way in finding new vaccines for diseases that currently do not offer adequate commercial incentives for pharmaceutical companies. Simultaneously Gavi and our global health partners continue to work hard to expand vaccine stockpiles in proportion to the risk of an outbreak.

The yellow fever vaccine. Photo credit: PAHO
Overall, vaccines have already achieved so much, but we still have a way to go to fulfil their potential of preventing diseases among the poorest and most vulnerable communities. In our complex and inter-connected world, immunisation also has other roles to play that can directly support the future of global health and development. And as we progress towards that future, it will be critical to keep this broader conversation going, ensuring we make the most of these remarkable live-saving tools.
This post originally appeared on LinkedIn.