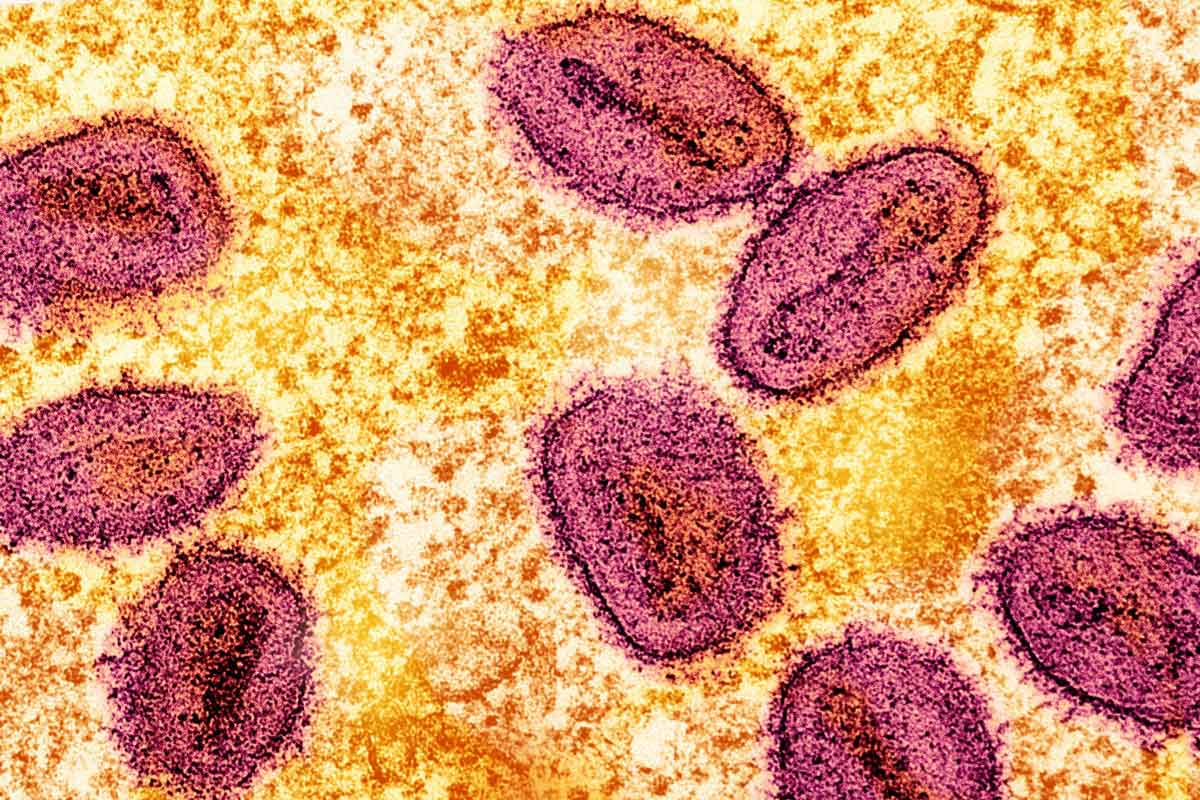
Meet the African scientists fighting the spread of mpox
Professor Dimie Ogoina was among the first to raise the alarm as mpox spread through Nigeria’s cities in 2017. VaccinesWork spoke to him and the DRC researchers tackling the latest outbreak.
- 17 July 2024
- 6 min read
- by Wealth Okete
Until 2017, Professor Dimie Ogoina’s experiences with mpox were strictly theoretical. But all that would change in September of that year, when he encountered his first clinical case of the disease in an 11-year-old boy at the Niger Delta University Teaching Hospital (NDUTH) in Bayelsa, Nigeria.
It was Nigeria’s first confirmed case of the disease since 1978, but also the beginning of an unfolding outbreak. By December, Ogoina had managed a sizable proportion of the over 200 cases reported across the country that year – and the majority of his patients were young, male adults, aged between 20 and 40.
Although worrisome, the observation that the mpox virus could infect young adults sparked Ogoina's curiosity, especially because the disease had been historically reported in young children. But that was not all he found out.
“What was also remarkable was that majority of those people [the young male adults] that presented with mpox had unusual lesions or skin rashes around the genital area, with ulcers. That seemed very unusual,” he says.
This unusual finding stoked his curiosity further, setting him on a long path of learning, which would lead to both new discoveries, and the enduring scrutiny of the scientific community. It also laid the foundation for his proposition that mpox could be transmitted via sexual contact.

While Ogoina’s work was largely based on the Clade II virus, common in West Africa, his findings have continued to inform responses to mpox outbreaks across the world.
In 2023, Ogoina was listed as one of Time100 Most Influential Persons, in recognition of his work on mpox, which by that time had garnered much global attention.
Challenges hinder efforts to tackle mpox
Mpox is a zoonotic disease, with the potential for both animal-human and human-human transmission. Although various animal reservoirs, including squirrels, rats and monkeys, may contribute to the disease's spillover into human populations, the exact transmission cycle remains an unsolved puzzle.
Since the first case surfaced in 1970, numerous mpox outbreaks have been reported in the Democratic Republic of the Congo (DRC), driven mainly by the Clade I strain of the virus. Unlike the Clade II mpox virus, which caused the global outbreak of 2022, the Clade I strain presents with more severe symptoms, with up to 10% fatality.
In a recent correspondence article published in Nature Medicine, the authors wrote that mpox “is emblematic of the global neglect of diseases that are endemic to Africa, up until they threaten the health security of the Global North. Progress must be made to control this disease and gaps need to be addressed to achieve global health security.”They highlighted gaps in laboratory testing and timely access to diagnostics, treatments, and vaccines as the key factors driving the spread of mpox in DRC, and by extension, Africa.
In an interview with VaccinesWork, Dr Daniel Mukadi-Bamuleka, who researches mpox and other emerging diseases like Ebola in the DRC, added negligence, low interest and limited funding to that list.
The need for more investment is still huge
Between April 11 and 13, a “High-level Emergency Regional Meeting on Mpox in Africa” was held in Kinshasa, DRC. The event offered a platform for discussing mpox epidemiology, strengthening collaborations between key stakeholders and partners, such as CEPI, WHO and UNICEF, and developing a robust action plan for tackling the disease in the continent. During this meeting, WHO and its partners committed to providing diagnostic and treatment packages to care facilities in remote areas to ensure a more decentralised and timely response to the ongoing outbreak.
Dr Beatrice Umba di Nguete, Technical Coordinator at the CDC/Kinshasa School of Public Health (KSPH), reflecting on the progress made during the meeting, says, “The need is still huge, but efforts are ongoing.” Dr Placide Mbala-Kingebeni, who was also present at the meeting, says that mixed teams pooled from the Ministry of Health have been deployed to conduct active disease surveillance, including the investigation of cases linked to sexual transmission, in affected regions. Mbala-Kingebeni, an associate professor at the University of Kinshasa medical school, heads the Epidemiology and Global Health Department, at the INRB (Institut National de la Recherche Biomédicale), DRC. Although these interventions have the potential to pave the path towards progress, he adds that limited funding continues to hamper the efforts of on-the-ground scientists.
Sexual transmission
WHO first issued a notification about the sexual transmission and emergence of Clade I mpox virus in new provinces across DRC on 3 November 2023. Although sexual transmission of mpox may no longer surprise scientists, it once did: before 2017, when Ogoina first began to observe a new kind of mpox in the patients he managed at his university teaching hospital. These patients did not only differ in their demographics, being young male adults, but also exhibited symptoms uncharacteristic of the classical mpox. Instead of a generalised rash, they presented with genital rashes and ulcers, and were frequently co-infected with sexually transmitted infections, like HIV or syphilis.
When Ogoina proposed that this new mpox, with the potential for sexual transmission, was at large, the scientific community doubted the veracity of his claims. But he was convinced of the hypothesis he made from these observations, describing them as “too remarkable to be ignored.” On July 23, 2022, WHO declared mpox a Public Health Emergency of International Concern (PHEIC), after it began to emerge in new regions across the globe. Similar to Ogoina’s earlier observations, cases were largely reported in men, and most of these men identified as gay and bisexual.
Vaccines, diagnostics and therapeutics to stem outbreaks
While the world has recovered from the 2022 mpox outbreak, DRC continues to grapple with the burden of a disease that never seems to go away. As at 26 May, 7,851 cases and 384 deaths had been reported from mpox across 177 of 519 health zones and 22 of 26 provinces in the DRC. More recent data from Africa CDC says 97% of the 8,479 cases reported across seven African countries so far, as at 14 June, are from the DRC.

The growing number of cases of the disease aside, Mbala-Kingebeni, who has been researching mpox since 2008, says significant progress has been made in recent times. “There are more cases detected because we now have capacity to diagnose directly in the field. We have a Gene Xpert and cartridges available, so we are able to diagnose rapidly and provide supportive care.” He adds that an ongoing clinical trial, led by the INRB and the NIH, is testing the effectiveness and safety of tecovirimat, an antiviral drug originally developed for smallpox, against mpox. Findings are expected to become available later in the year.
Results from a now-completed mpox vaccine trial in health care workers are also promising. However, there is a need for an efficacy study to validate them. He anticipates that the study could be conducted by 2025.
The way forward
Despite these many interventions, it is unlikely that the disease is going to be eliminated soon. The absence of serological point-of-care tests, therapeutics and vaccines, alongside poor health-seeking behaviours, weak surveillance systems and obscure animal reservoirs complicate the ongoing fight. While increased investments in mpox research and development could address these issues, Ogoina also strongly advocates for improved awareness about the sexually transmitted new mpox – naturally without neglecting classical mpox.
Eliminating or eradicating mpox may not be in sight, but vaccines remain key to breaking the chain of transmission, fighting off infection and preventing disease in endemic regions, argues Mbala-Kingebeni.





