How One Health can help ease climate-driven health crises
As extreme heat awareness rises, a One Health approach and robust adaptation strategies are essential for climate-resilient health systems.
- 16 July 2024
- 6 min read
- by World Economic Forum

- There is growing awareness of extreme heat's detrimental effects on health and livelihoods, with initiatives like the first Heat Action Day on 2 June.
- A comprehensive One Health approach is essential for addressing interconnected health crises amplified by climate change.
- Adaptation strategies in building climate-resilient health systems are critical, including optimizing healthcare systems for extreme weather events, enhancing global monitoring for disease outbreaks and developing comprehensive risk assessments and response plans.
It’s official. Heat is now firmly on the agenda and in the public consciousness. The second of June was the first Heat Action Day, raising awareness of the detrimental impacts of extreme heat on lives and livelihoods after a report found that 26 days of the hottest 12 months on record were “excess” heat days likely due to climate change.
The impact of unprecedented heat during high-profile events, such as the Tokyo Olympics in 2021, has also raised concerns about how it will impact future Games, including the Paris Olympics this summer.
As elite tennis player Novak Djokovic noted in Japan, the conditions were tougher than anything he had experienced in his decades-long career: “You’re constantly dehydrated; you feel you have weights on your shoulders because there’s so much heat and humidity and stagnated air.”
Those impacts can be even starker among the young, old, poor and those obliged to work outdoors, as mentioned in a report earlier this year involving the Red Cross Red Crescent Climate Centre. However, heat is one aspect of the myriad effects of climate change that impact disease spread and health infrastructure.
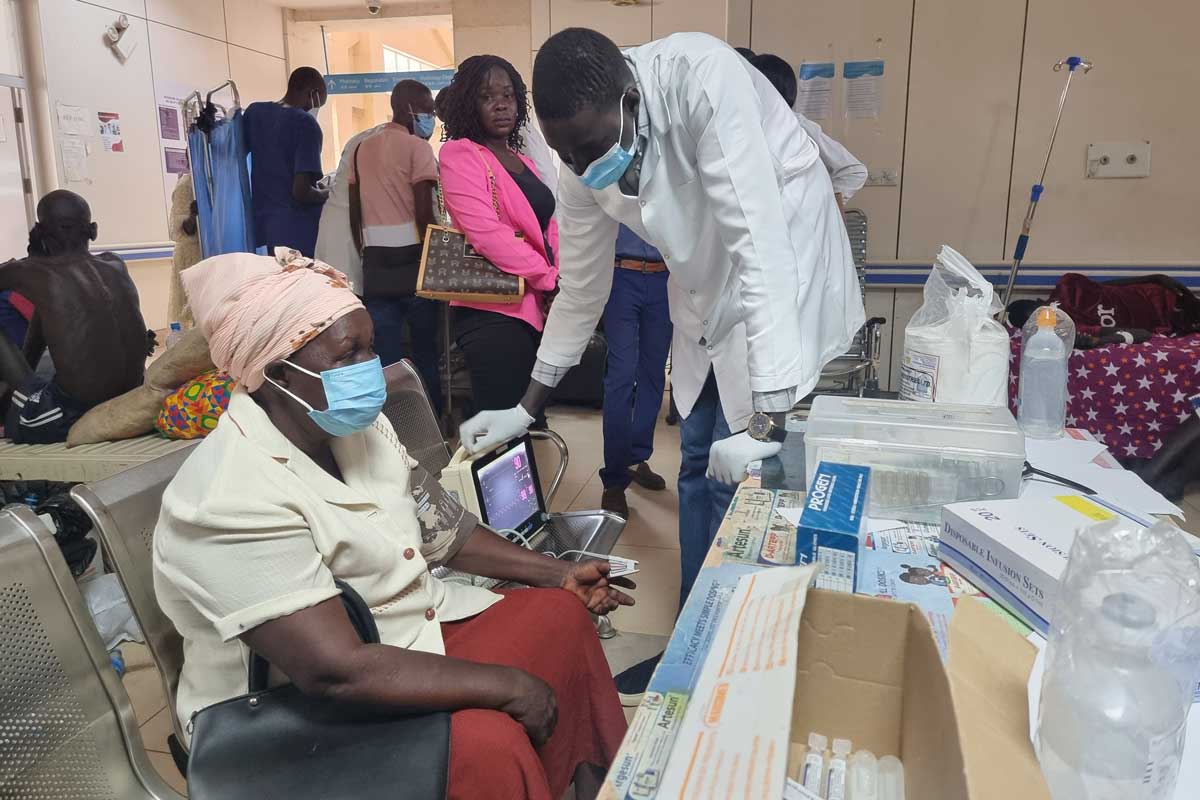
Due to the expansion of mosquito habitats, the increase in pollution-related illnesses and vector-borne diseases such as dengue, malaria and Zika necessitate different health care services. By 2050, climate change is projected to cause 14.5 million deaths and $12.5 trillion in economic losses, with low- and middle-income countries disproportionately affected, having already incurred 91% of deaths from climate-related events in the past 20 years.
Have you read?
That’s why a comprehensive and holistic One Health approach is crucial in effectively addressing the interconnected health crises amplified by climate change, with a strong focus on adaptation strategies to mitigate the impacts on global health systems.
Action is required and it must be swift.
One Health approach
The first priority is a radical change in mindset worldwide. Governments across the Global South and North must adopt a One Health approach, which recognizes the connection and interdependence of the health of people, animals and ecology. The One Health approach seeks to balance and optimize the health of each, protecting them from the effects of climate change while recognizing their interdependence and the resulting impact.
In practice, applying a One Health approach means that all actions to prevent, predict, detect and respond to health threats should consider the interlinkages between human, animal, plant and ecosystem health.
For example, the approach requires researchers and risk assessors to integrate and share knowledge from different disciplines (e.g. veterinary, environmental and human health sciences) when assessing the health risks posed by certain disease vectors or contaminants. It also requires risk managers and policymakers to address the source to prevent and mitigate risks to health, for instance, by reducing human pressures on the environment.
In Southeast Asia, there have been recurring episodes of avian influenza outbreaks. A comprehensive One Health strategy was embraced, fostering collaboration between the animal and human health sectors to monitor and manage the disease. Measures included eradicating infected poultry, administering vaccines to birds and bolstering surveillance systems. This coordinated response helped suppress further outbreaks and spread of the virus to humans.
Also, a proactive approach to combating antimicrobial resistance in the European Union involved a One Health strategy, leading to the establishment of the European Antimicrobial Resistance Surveillance Network.
The network collects and analyzes data from the human health, veterinary and environmental sectors to track and address trends in antimicrobial resistance. The cooperative approach has significantly improved antimicrobial resistance management and helped promote the responsible and prudent use of antibiotics across sectors.
“Businesses have prioritized reducing their carbon footprint over climate adaptation, with only 27% viewing adaptation as a high priority compared with 60% for mitigation.”
Adaptive strategies
Adaptation is a key facet of the One Health approach but can take several forms.
1. Preparing for extreme weather
Health care systems and practitioners should be prepared for extreme weather events as these typically increase the demand for health services while often undermining the availability of those same services.
Adaptation at this level is also multifaceted, including the design of health care facilities. For example, can electricity, heating and ventilation be assured following widespread flooding? This phase requires cross-sector and professional consultation, such as with experts in climate change, building design or land use.
China’s “sponge cities” are a promising example of an adaptation strategy created to enhance urban water management by increasing the permeability of city surfaces, creating green spaces and using materials and designs that absorb and reuse rainwater.
2. Policy, and resourcing around health effects
Extreme heat is a prime example of how policymakers can mitigate the health impacts of climate change. Early warning systems can alert populations to impending climate events, such as heat waves, allowing for preparatory measures.
Several big technology companies, including Microsoft and Google, are collaborating with the World Meteorological Organization to improve alerts, internet speeds, disaster forecasting and response using AI and satellite technology.
Health systems must be able to swiftly stabilize populations and infrastructure after extreme weather events and provide long-term treatment for conditions such as smoke inhalation and trauma following wildfires and other similar incidents.
3. Anticipating outbreaks
Adaptation can also involve preparing health care services for a pandemic or specific disease outbreak due to climate change. Measures might include:
- Enhancing global monitoring systems.
- Improving communication and education.
- Conducting vaccination research.
- Understanding what control measures will serve an outbreak.
However, businesses have prioritized reducing their carbon footprint over climate adaptation, with only 27% viewing adaptation as a high priority compared with 60% for mitigation. Moreover, the COVID-19 pandemic highlighted how reduced workforce capacity can impact productivity and supply chains, underscoring the need for more analysis of sector vulnerabilities to climate shocks.
Climate-resilient health systems
Preparation, adaptation and mitigation will also take place as comprehensive risk assessments, response strategies and control plans are developed to monitor and address climate-related health issues, such as the spread of mosquito-borne diseases.
Successful past responses to health crises, such as the SARS outbreak in 2002 and the cholera outbreak in Mozambique, highlight the importance of coordinated international efforts. Creating a climate-resilient health system requires adaptation planning, research, continuous evidence gathering, capacity building and clear policy making.
Innovative public-private partnerships can also fill a gap where vulnerable populations can better use predictive data that’s within their reach, including on heat waves. The Forum’s multi-sectoral Climate & Health initiative is dedicated to developing these adaptation strategies and improving the management of the intricate relationship between climate impacts, ecosystems and health infrastructure.
So now that heat is on the agenda, we can view it as part of an integrated strategy to mitigate climate change harm for which we all bear responsibility.
More from World Economic Forum
Recommended for you