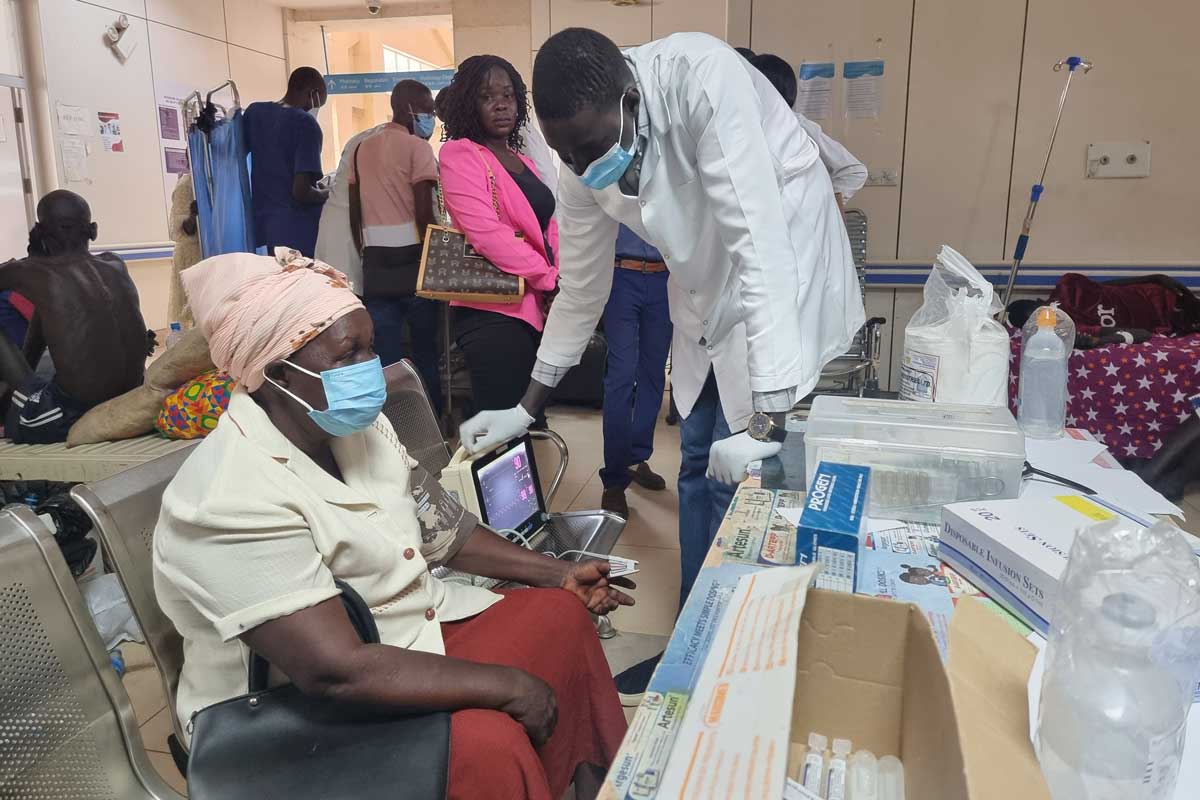
With early evaluations of combined immunisation and hygiene programmes showing promising results, more research is needed into what could make a huge difference to health in low- and middle-income countries. Sophie Durrans, Research Uptake Officer at the SHARE Consortium, and Megan Wilson-Jones, Policy Analyst – Health and Hygiene at WaterAid UK, examine the connection.
Water, sanitation and hygiene (WASH) and vaccination are each important tools in the prevention and control of disease, including of common childhood conditions such as diarrhoeal diseases.
Long-term, comprehensive disease control and prevention requires safe, clean and adequate water and sanitation infrastructure and sustainable hygiene practices in addition to vaccination programmes; these must exist alongside many other critical factors including disease surveillance and strong health systems that reach everyone.
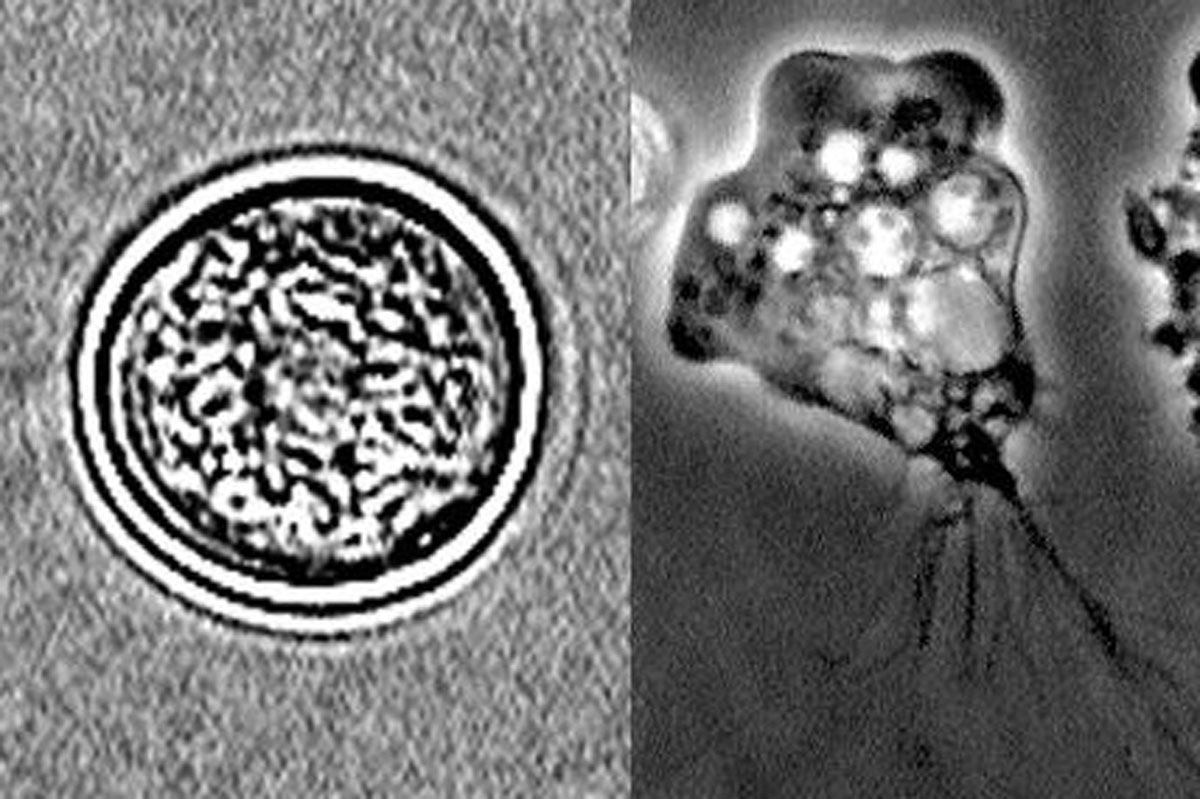
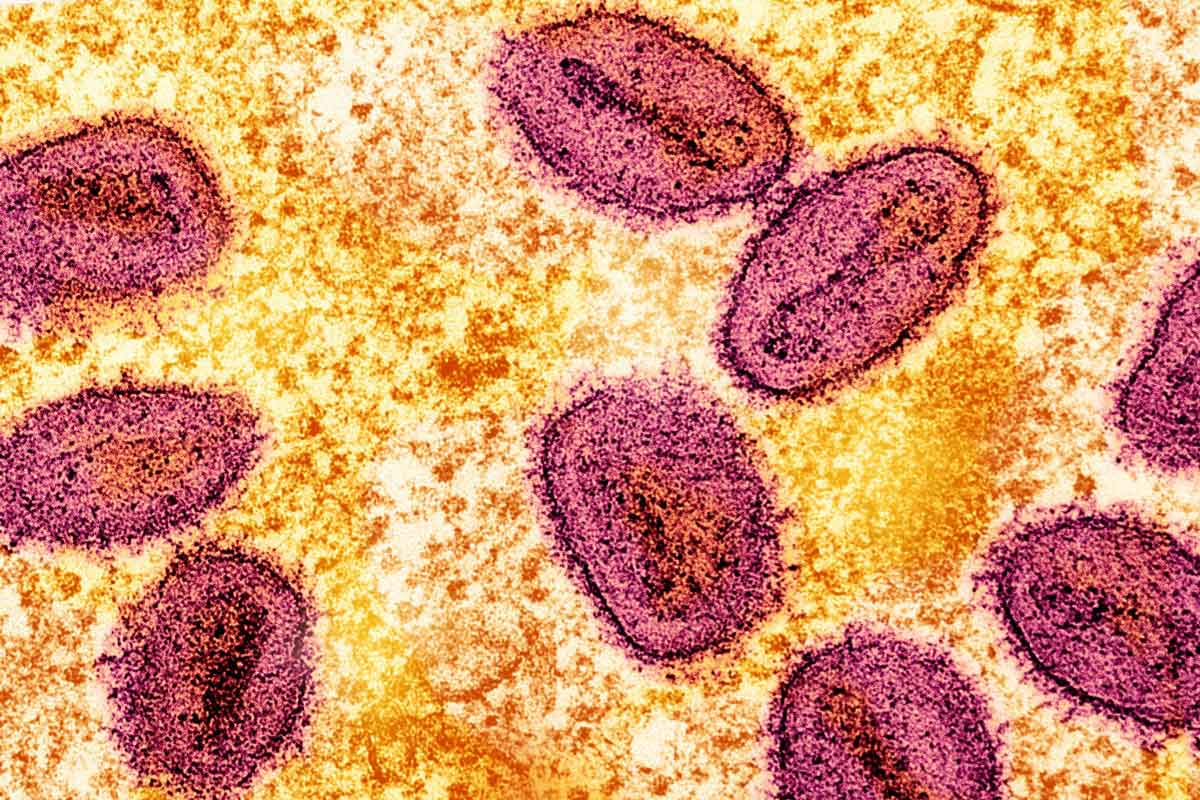
Compared with injectable vaccines, live oral vaccines can better protect against intestinal infections and are often easier to deliver at scale and to remote communities. However, the effectiveness of oral vaccines differs significantly by region and country. For example, the same rotavirus vaccine that protected 98% of children in the USA and Finland only protected 43% of children in Bangladesh.
This lower effectiveness is often seen in many low- and middle-income contexts, where the burden of vaccine-preventable diseases is highest. The difference in vaccine effectiveness by region is not a new phenomenon – variations have been noted since the early oral polio vaccine trials in the late 1950s.