Following last week’s launch of “Ending Cholera: a Global Roadmap to 2030”, we spoke to Allen Maina, Senior Public Health Officer at the UN High Commissioner for Refugees (UNHCR), about the difficulties of tackling cholera in displaced populations and the significance of this global call to action.
How ambitious is this goal to end cholera by 2030? What do you think the main hurdles will be?
The feeling right now is that at face value it’s an ambitious goal, but achievable, because there’s a strong resolve to end cholera. The impact is visible and the solutions to ending cholera are also known. There is a great advancement in evidence and more has come out rapidly in the last year. I think with this kind of momentum it’s possible to achieve the target to end cholera by 2030. The main hurdles will be anyone who may politicise the “End Cholera” project. If it’s seen for what it is – about saving lives – I think it will be very much achievable. The main hurdle will be getting the political commitment for its implementation.
How will displacement due to conflict and natural disaster affect the incidence of cholera?
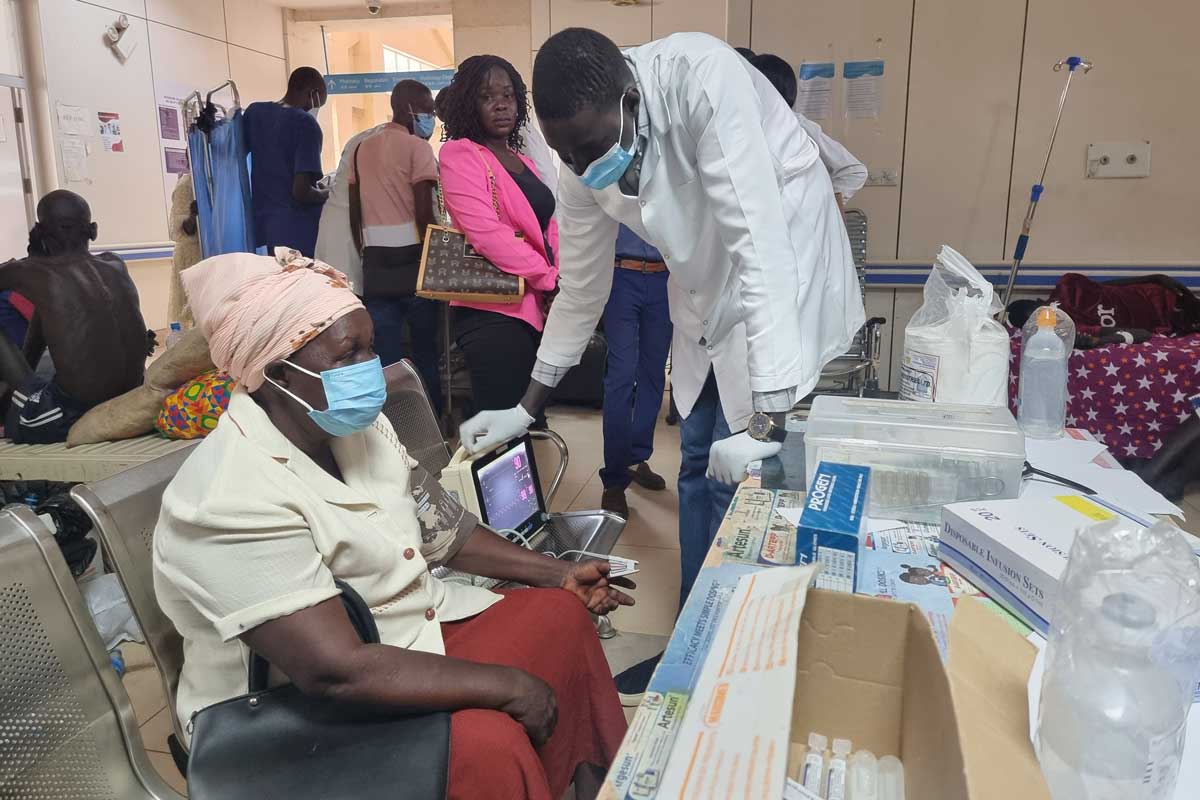
This depends on where the displacement is occurring. In many countries in Africa for example, and in some Asian contexts, the endemicity of cholera would be of a grave concern. Thinking about the current example, Bangladesh, this is mainly because people are living in very congested conditions. It’s difficult to set up appropriate sanitation facilities in complex emergencies associated with large movements. Even for simple latrines the emergency standards are hard to achieve. Therefore crowding and poor sanitation conditions in an acute stage of a displacement are significant concerns.
How will this make the elimination of cholera more challenging?
If you don’t respond fast to an acute emergency in a high cholera outbreak risk context, cholera will strike. It then becomes very hard to contain. The important thing to realise is that cholera must be controlled not just in the refugee setting, but also in the host communities. You can’t just concentrate on a refugee setting without including the host community and the wider district, including markets, where cholera can spread.
How important will vaccines be in achieving this?
Vaccines will be an important element in reducing morbidity and mortality related to cholera and there is evidence to show that. If you get the population vaccinated immediately at the onset of an emergency as preventive measure, if cholera outbreaks occurs, it will quickly be brought under control. This is because you already have herd immunity, meaning most of the population is already protected through vaccination. This allows time to set up proper water and sanitation facilities and ensure education of the community on proper hygiene.
Therefore oral cholera vaccine (OCV) has a significant impact and is easy to implement in refugee emergencies. If people are organised in a camp it’s easier to reach them. If they are living among villages it makes it harder but it’s still possible – we’ve done it in such settings before.
Could you give an example?
I can give two: one where we responded to prevent cholera and another where oral cholera vaccine (OCV) was used to contain it.
Firstly, in 2014 there was an influx of refugees from South Sudan into the Gambella region of Ethiopia. In Gambella at that time there had been no cholera reported for years, but we knew there was cholera in South Sudan. Together with MSF, WHO and the national health partner (ARRA) we were able to make a strong case for oral cholera vaccination of the refugee population and surrounding host communities. If cholera came it could be contained – we wanted to make sure we were ahead of the curve. Through some good joint advocacy with partners and donors, we were able to get it approved and the Minister of Health supported it. We implemented it, and no cholera cases were reported during that acute emergency.
The second example is in Tanzania, where we had a cholera outbreak. This was an emergency in 2015 with refugees coming from Burundi, and we had a cholera outbreak around Lake Tanganyika. It was spreading very fast. We conducted an oral cholera vaccination campaign for the refugees and the surrounding communities. Cholera was brought under control in a month. Incidence was dramatically reduced, and deaths decreased.
Why do you think there hasn’t been a call to action like this before?
That’s a good question. I don’t know. I think it’s more related to the fact that now we have some good solutions to getting ahead of the curve – particularly the oral cholera vaccine. It has added an extra element to the control of cholera. This year, we have brand new evidence that shows the strong impact of using oral cholera vaccination. I think that momentum has resulted in a need to say: ‘Hey, guys, it’s actually possible to get cholera under control, and let’s have a global call to action and build on that momentum.’
Find out more about Gavi’s work supporting oral cholera vaccines here, or read more about the Global Roadmap to end cholera by 2030. Read more about the work of UNHCR here.