WHA77: 50 years of immunisation history light the way forward
The first half-century of routine vaccination saved 153 million lives. That calls for optimism, even in the face of sobering challenges.
- 23 May 2024
- 8 min read
- by Pascal Barollier
Gavi at the 77th World Health Assembly
Download Gavi's high-level messages to learn more about our key recommendations for this year's delegates:
English | French | Portuguese | Spanish
Gavi is hosting and participating in several World Health Assembly side-events. See the full list here:
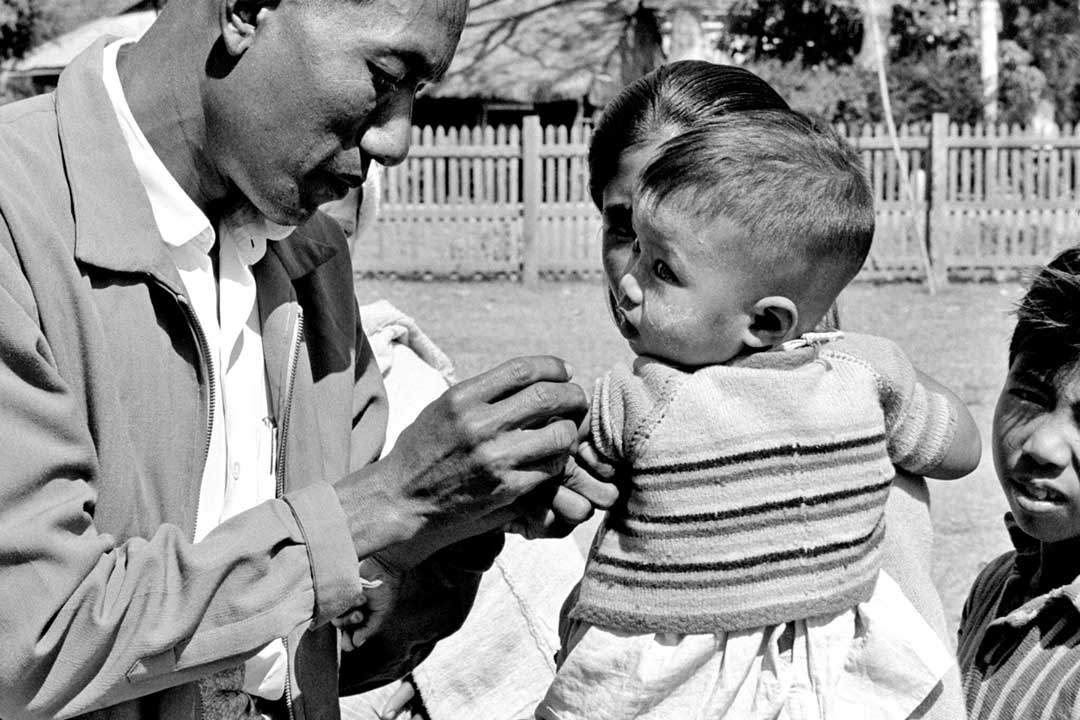
Monday morning, 20 May 1974: ABBA’s Waterloo is looping on Swiss radio as delegates to the 27th World Health Assembly shuffle into their conference hall seats at Geneva’s Palais des Nations for the session’s tenth meeting. An ambitious proposal, tabled jointly by the delegations of the Netherlands, Ethiopia, India, Poland, Qatar, Somalia, the USA and Venezuela1, is before them.
It calls for what is being referred to as an expanded programme on immunization. Specifically, the draft resolution recommends that “Member States not currently having adequate vaccination programmes develop plans to include in their health services immunization and surveillance against some or all of the following diseases: diphtheria, pertussis, tetanus, measles, poliomyelitis and tuberculosis.” The phrase, “and others, where applicable” will be added, with commendable foresight, during the deliberations.
The principle meets with support from the floor: the eradication campaign against smallpox is nearing triumph, fuelling enthusiasm. Immunisation, says Dr WB Gerritsen of the Dutch delegation, is acknowledged as the quickest and most effective measure of preventive medicine – but in “extensive regions of the world,” it remains available to only a small proportion of children.
Dr Wang Kuei-chen, a “barefoot doctor” from China, attests from experience to the transformative potential of vaccines as part of a programme of primary health care. Dr Kupferschmidt of the German Democratic Republic likewise reflects on the precipitous drop in childhood deaths from polio, measles, tuberculosis and tetanus that his own country has witnessed in the last 29 years. Professor J Kostrzewski, an adviser to the team from Poland, urges that immunisation should be “one of the most important future activities” of WHO.
Dr Widad Kidane-Mariam, chief delegate from Ethiopia notes, regretfully, that instituting an immunisation programme like the one that is central to her own country’s health system remains beyond the means of many other developing nations. Tanzanian delegate Dr E Tarimo, says that measles is the priority problem in his country, as in many others, and calls on WHO to coordinate a global fight against the viral disease. “More stable” and “less expensive” vaccines are needed, he says, but meantime, “more aggressive measures” should be used to deploy the vaccines that exist.2
The idea is welcomed, but the text is complicated and imperfect, and deliberations must continue. That afternoon, the WHO Virus Diseases Programme's Dr WC Cockburn will contribute for consideration that in many countries just 10–20% of children have “any hope” of vaccination against diphtheria, pertussis and tetanus – fewer still against polio or measles.
Perhaps the formal language and stiff rhythms of formal diplomacy have, at moments, camouflaged the colossal scale of the project under discussion, but Cockburn’s interjections surface it again.
Have you read?
Seventy million children turn one year old each year in the countries under discussion; reaching 80% of them would mean vaccinating 56 million children every year. There “is no foreseeable end of the use of the vaccines in question,” he says. The proposed programme, once begun, “must be continued”.
On Wednesday afternoon, a commitment at last: the resolution is approved. On Thursday, Professor A Pouyan of Iran, presiding over the session’s closing, celebrates the decision: “The prospects offered by immunisation for more effective control of the communicable diseases are scientifically justified and borne out by the results already obtained with some of those diseases,” he says.
2024: “Borne out by the results”
Half a century has passed. The delegates to the World Health Assembly are once again, for the 77th time, preparing to take up their seats at this most important decision-making forum in global health. The EPI – once the Expanded Programme on Immunization, now the Essential Programme on Immunization – is a venerable 50 years old. In that time, vaccination has saved 154 million lives.
154 million lives: that’s more than 3 million lives each year, or six lives every minute. A child born this year is 40% more likely to live to their next birthday than a child born in 1974. And, since 2000, when Gavi was established, heralding another tremendous bump in vaccination rates in low-income countries, the global under-five mortality rate has declined by 51%.
154 million lives have been saved by vaccination in the 50 years since the EPI was signed into existence at 1974’s World Health Assembly. Since 2000, when Gavi was established, the global under-five mortality rate has declined by 51%
Bet on equity, bet on prevention
But despite that staggering progress, the health leaders gathering in Geneva will be painfully aware that more needs to be done in the names of both global health security and equitable access to essential services.
The COVID-19 pandemic hit health systems hard, and despite the muscular catch-up efforts carried out by many national immunisation systems in the wake of 2020’s forced disruptions, 14.3 million children still didn’t receive a single dose of any vaccine in 2022. The upshot of declining coverage has been as predictable as it has been hard to witness: 43% more people died of measles in 2022 than in 2021. Diphtheria, pertussis, polio and other previously quietened foes have resurged in various countries.
If vaccination was preventive medicine’s best bet in 1974, that’s patently only truer now, equipped as we are with a larger – and still expanding – arsenal of life-saving vaccines, and data that reveals the durable and rippling benefits of vaccinating children as routine. Today, immunisation is often a child’s first point of contact with the health system – a portal, as such, to accessing care in general. Reaching unimmunised zero-dose children with vaccines might grant them their only shot at an adult life. It might, moreover, offer them a pathway to a fairer one.
In 2024, there are newly winnable battles on our horizons. The HPV vaccine, for instance, brings the elimination of cervical cancer within reach; investment in the introduction of malaria vaccines promises to make a colossal dent in mortality rates from this leading killer of children. Tomorrow, 43,200 doses of the brand-new R21 Matrix-M vaccine will touch down in Bangui, ready to kick off the Central African Republic’s first-ever immunisation campaign against the mosquito-borne scourge.
![[16:00] Maya Prabhu (Consultant) Six-month-old Fiona waits to get vaccinated against malaria at the Soa District Hospital in Cameroon.](/sites/default/files/vaccineswork/2024/Body/RS50824_VBE_2990_h2.jpg)
Credit: The Global Fund/Vincent Becker
Echoing Dr Tarimo, Tanzanian delegate to WHA27, we call for both investment in more and better vaccines, and investment in “more aggressive measures” to deploy the ones we have. The progress of the last 50 years guides our optimism
Like Dr Tarimo of Tanzania, whose country’s measles rates were already dipping just seven years after he spoke in Geneva, a brief six years after the Tanzanian EPI began operations, we urge both investment in more and better vaccines, and investment in “more aggressive measures” to better deploy the ones we have.

Credit: Gavi/2014/Karel Prinsloo
This call for investment in immunisation couldn’t be more topical, with Gavi set to launch its 2026–30 Investment Opportunity at The Global Forum for Vaccine Sovereignty and Innovation, due to be held in Paris on 20 June. This event will set out why immunisation deserves continued support from donors across the world over the next five years.
Prepare for the coming shocks
There will be more pandemics, and that knowledge must inform policy. Discussion of Pandemic Prevention Preparedness and Response (PPPR) at WHA77 must acknowledge the need to strengthen national primary health care and preventive services to meet the coming challenge, alongside arranging for financial and technical instruments to ready a concerted global response.
There is also no doubt that climate change and antimicrobial resistance are advancing, mounting a twin challenge to established health care paradigms. We urge the WHA delegates to adopt and implement the proposed WHA resolutions on climate and health, and antimicrobial resistance. At national level, mitigation measures against these threats need to be integrated in National Action Plans and implemented with preventive health measures.
Vaccines: a key tool to tackle antimicrobial resistance (AMR)
The challenges, we realise, are big, and growing. But the achievements of the last 50 years show us the colossal scale of what’s possible.
Find us at the World Health Assembly
Mark your calendar, and join Gavi at the following WHA77 side-events.
Monday, 27 May
- Eliminating Outbreaks Through Prevention, Detection and Coordination – This Gavi event, co-hosted with UNICEF and the Bill & Melinda Gates Foundation, will highlight the central importance of vaccines as a tool for outbreak prevention, detection and response, as well as financing to support immunisation partners in this area of work.
- Devex Checkup at WHA77 – Devex will convene global health leaders for an in-person event in Geneva that will highlight the policy, resources, and partnerships necessary to accelerate progress on global health goals. Register here.
Tuesday, 28 May
- Immunising in Fragile and Conflict Settings: Challenges and Opportunities – This Gavi-hosted side-event will shed light on what it means to work in fragile and conflict settings, the approaches that are effective in driving immunisation coverage, and how they should be tailored for maximum impact – including zero-dose children who have not been reached by routine immunisation services. Register here.
- Celebrating 50 years of immunisation progress: honouring achievements, embracing innovation and envisioning the future – This event will honour and celebrate achievements in immunisation over the past 50 years, take stock of what we’ve learned and collectively set ambitious goals for the next 50 years of essential immunisation programmes.
Wednesday, 29 May
- Strengthening PHC: Combining Immunisation and Nutrition to Improve Children’s Health – This side-event will share best practices for a combined approach within PHC services, using lessons learned from immunisation and nutrition integration (INI). Register here.
Thursday, 30 May
- Foreign Policy Global Health Forum – This event will bring together leaders across the global health community to reassess priorities, forge new partnerships, and commit to actions that will address current disparities and fortify the world against future health crises. Register here.
- In the course of proceedings, the delegations of Austria, Ecuador, Ghana, Cameroon and Tanzania would request to be listed among the resolution’s co-sponsors
- Thailand’s Dr Hemachudha suggests that bulk purchases of vaccine by developing countries might enable a drop in vaccine prices, facilitating an expansion in immunisation programmes. We think that’s a great idea.