How rotavirus vaccines are changing the game
Rotavirus vaccines have proven to be a cost-effective intervention that not only saves lives, but also reduces the burden on families and health systems.
- 24 April 2025
- 3 min read
- by PATH

World Immunization Week, celebrated the last week of April, is a chance to reflect on the immense success that vaccines have had in improving child health and easing the burden of disease for families, health care systems, and governments. Rotavirus vaccines, first introduced in 2006, are a prime example of this achievement—and thanks to recent introductions in high-burden countries, their impact is poised to accelerate in the years ahead.
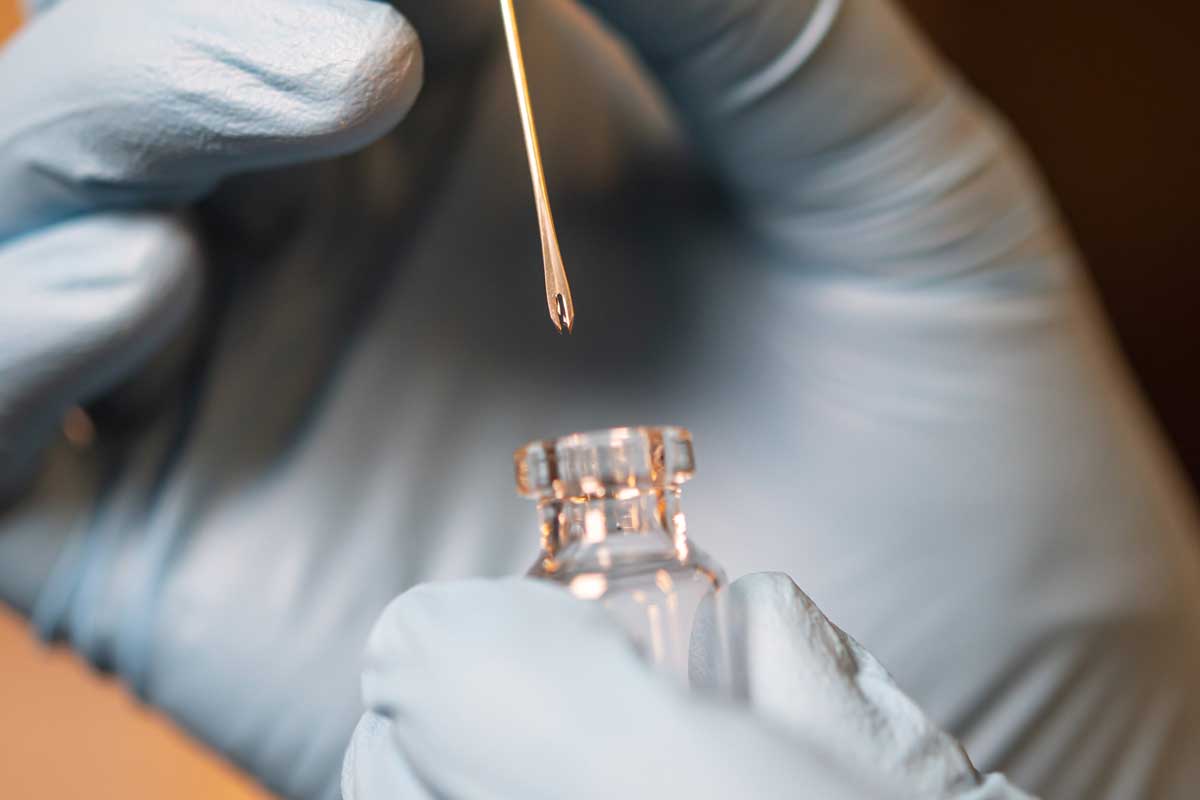
A new tool for diarrheal disease prevention
Rotavirus presents a unique problem: it spreads quickly and cannot be prevented by improvements in water, sanitation, and hygiene (WASH), unlike the bacteria and parasites that cause other forms of diarrhea. Before rotavirus vaccines became available, the disease was responsible for nearly half a million deaths each year, and almost every child had been infected before their fifth birthday.
That changed in 2006, when Nicaragua and the United States were among the first countries to introduce rotavirus vaccines. This milestone marked the first time a vaccine was introduced in both a low-income and high-income country simultaneously, closing an access gap that had often stretched for decades for other vaccines.
Rotavirus vaccine also helped facilitate greater momentum for integrated approaches to diarrheal diseases, an approach that was piloted in Nicaragua. When the vaccines first became available, rotavirus had low name recognition, but the burden of diarrhea on health systems was obvious. Communications efforts used this insight to increase uptake by putting rotavirus vaccines within the context of a toolbox of diarrhea interventions, alongside WASH, oral rehydration solution (ORS), zinc, nutrition, and breastfeeding.
Have you read?
The ripple effect of rotavirus vaccines
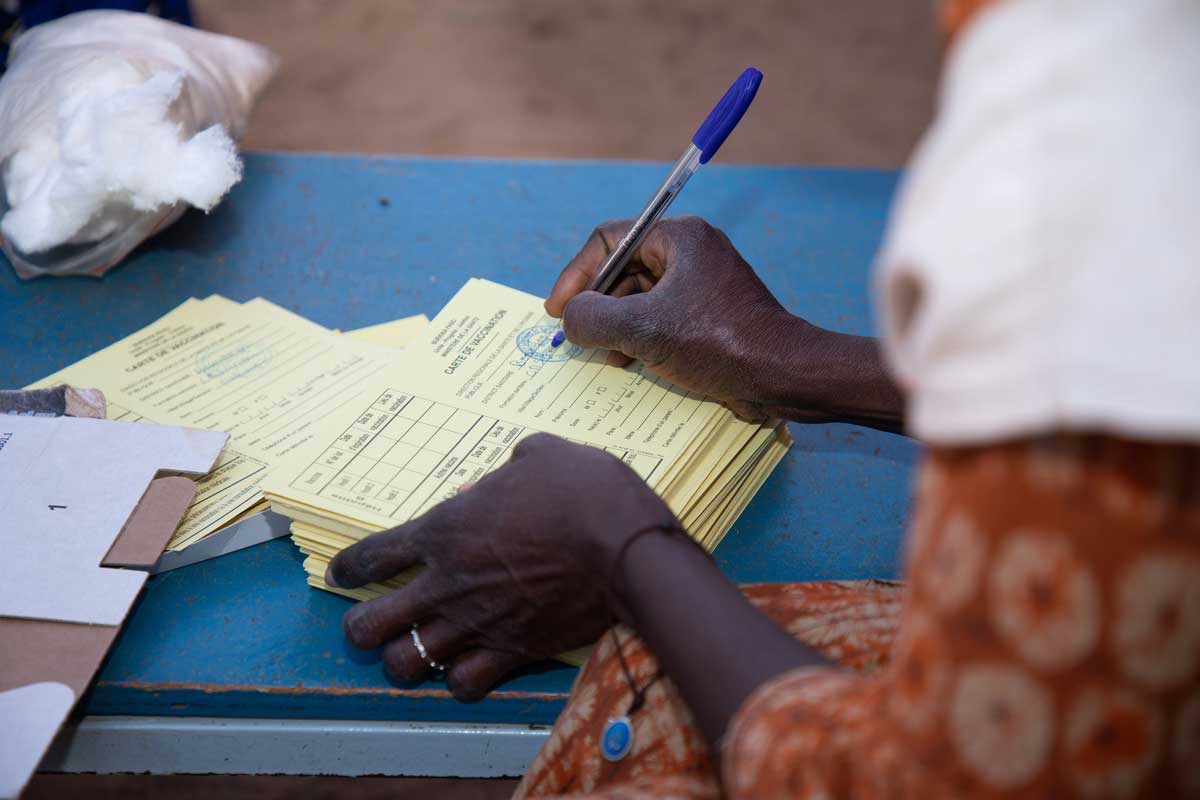
From 2006 to 2019, the vaccines saved an estimated 140,000 children’s lives, and that number has only grown since. Nigeria, a country with one of the highest burdens of diarrheal disease, introduced the vaccine in 2022, marking a major milestone for prevention and control. More than 120 countries have introduced rotavirus vaccines into their routine immunization programs, with more planning to do so this year.
Beyond lives saved, rotavirus vaccines are reducing the burden on families and health systems. Countries that introduced the vaccine observed a 59 percent average reduction in rotavirus hospitalizations among children less than five years old, and a 36 percent decrease in deaths from severe diarrhea. Every vaccine helps keep kids in school, prevents caregivers from missing work, and creates savings for health systems and governments that would otherwise have been spent on costly treatments.
A new report on DefeatDD.org goes deeper into this impact, compiling the available data on rotavirus vaccines into one resource. The report breaks down the effects of vaccine introduction at the global and national level, from averting hundreds of thousands of deaths to saving millions in treatment costs.
Over nearly two decades, rotavirus vaccines have proven to be a cost-effective intervention that not only saves lives, but also helps keep families from potentially crippling financial hardship. Vaccines are one of the best investments we can make in public health—and when it comes to rotavirus vaccines, we’re already seeing the returns. As more countries introduce rotavirus vaccines, and as those that have already done so work to improve coverage, continued investment in immunization will be essential.
Click here to read the full report on the impact of rotavirus vaccines.