Introduction
According to the World Health Organization (WHO), “antimicrobials – including antibiotics, antivirals, antifungals, and antiparasitics – are medicines used to prevent and treat infectious diseases in humans, animals and plants”.1 Antimicrobial resistance (AMR) is a natural process that occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective, and infections become difficult or impossible to treat – thereby increasing the risk of disease spread, severe illness, disability and death.2
AMR is recognised as an urgent global health challenge, with drug-resistant bacterial infections causing an estimated 1.27 million deaths per year globally.3 AMR affects all age groups in all regions of the world, with low- and middle-income countries (LMICs) being most severely affected. AMR affects not only human health, but also animal health, food production and the environment, as well as contributing to increased health care costs and reduced economic development. In 2017, the World Bank estimated that, if not controlled, AMR would cause US$ 1 trillion to US$ 3.4 trillion annual losses to gross domestic product (GDP) by 2030 and an additional US$ 1 trillion in health care costs by 2050.4
Recognising the significant health care and financial burden of uncontrolled AMR, in 2016 the United Nations (UN) convened a high-level meeting on antimicrobial resistance that has resulted in greater attention being given to efforts to control AMR. However, persistent challenges remain in implementing the Global Action Plan on AMR. Infection prevention and control in human health has seen minimal progress since 2015, according to WHO’s 2021 review of the Global Action Plan on AMR.5
In September 2024, a second high-level meeting on AMR will be convened as part of the High-level Week of the UN General Assembly, in recognition of the continuing challenges and ongoing importance of tackling AMR at global and national levels. The theme of the high-level meeting will be “Investing in the present and securing our future together: Accelerating multi-sectoral, global, regional and national actions to address Antimicrobial Resistance”. This presents an important opportunity for countries and the global health community to secure political commitment for the integration of preventive health measures, such as immunisation programmes, in the package of interventions that are needed to tackle the burden of AMR.
AMR remains a significant health and development challenge and in 2021 was listed as one of WHO’s top ten global health issues to track. It is estimated that AMR contributes to 5 million deaths per year (including the 1.27 million directly attributable to AMR), 1 million of which are among children aged under five years.6 The number of children under five dying from drug-resistant diseases suggests that the potential benefits of vaccines are an important tool to protect against AMR are not being fully realised.
While vaccines had been mentioned in the Global Action Plan on AMR and included in the Political Declaration of the 2016 high-level meeting on AMR, the true value and potential of vaccines in preventing AMR were not recognised until recently. Analysis of 108 national AMR plans, for example, found that just 13% (or 14 out of 108 national action plans) included immunisation and the need for strengthening immunisation programmes as a tool for preventing and reducing AMR.7
Immunization Agenda 2030 (IA2030), however, clearly highlighted the contribution vaccines make to preventing AMR, stating that vaccines are “widely seen as critical for addressing emerging infectious diseases by … combatting the spread of antimicrobial resistance.”8 The accompanying action framework, ‘Leveraging Vaccines to Reduce Antibiotic Use and Prevent Antimicrobial Resistance’, clearly highlights that vaccines are effective tools to prevent infections, which can, in turn, make a major contribution to the prevention and control of AMR.9
Most recently, a WHO Resolution on AMR, proposed for agreement at the 77th World Health Assembly in May 2024, references the need for research and development for vaccines, diagnostics and treatments; and highlights the importance of implementing IA2030 as a key part of WHO’s global strategy on infection prevention and control.10
Despite this, vaccines continue to be undervalued as a tool to tackle AMR.
2. The prevention effect of vaccines
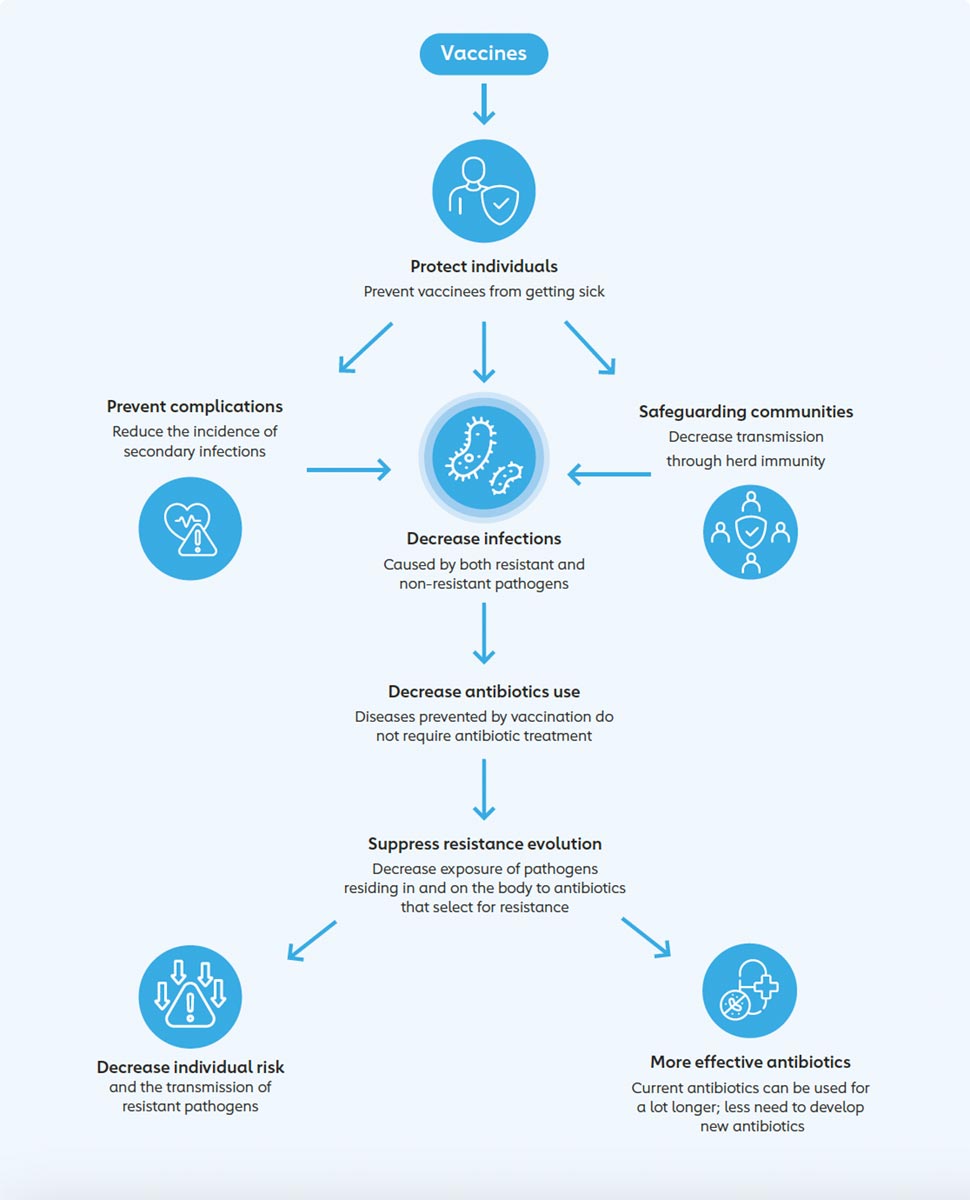
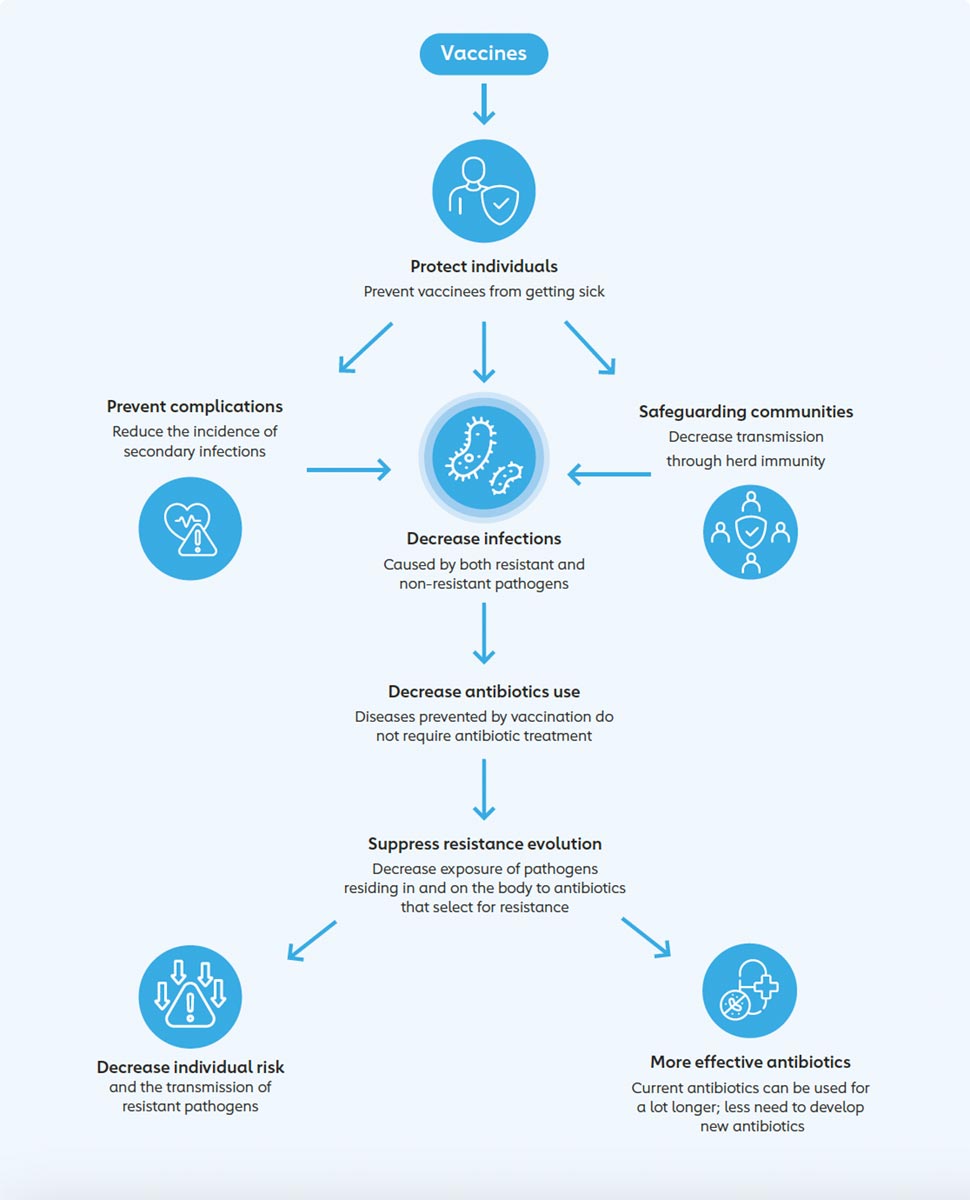
Immunisation decreases rates of infection and thereby antibiotic use, thus preventing the development of resistant infections. As such, vaccines are considered one of the most cost-effective ways of preventing morbidity and mortality, and are an important tool in tackling AMR. Three broad categories of vaccines have been identified as being useful to help contain the rise of drug-resistant infections:11
- Vaccines that prevent bacterial infections commonly acquired by the general population, often called ‘community-acquired infections’. These vaccines prevent bacterial infections by reducing carriage (the infection of an individual without causing symptoms) and thereby protecting individuals within a community, while also negating the need for antibiotics, reducing the opportunity for bacteria to develop resistance and reducing the transmission of antibiotic-resistant bacteria.
- Vaccines that prevent bacterial infections commonly acquired in hospital, often called ‘hospital-acquired infections’ (HAI). The impact of drug-resistant infections in health care settings such as hospitals can often be considered worst, due to the associated health implications for patients and the high risk for the spread of bacterial infections.12
- Vaccines that prevent viral infections. These vaccines are important because a large proportion of unnecessary prescribing of antibiotics occurs for patients who have viral infections, even though the drugs will not help in these cases.
More simply put, vaccines protect people from infection and reduce their spread, thereby limiting the opportunity for AMR to develop. High rates of immunisation can lead to herd immunity,13 further reducing the risk of infection and development of resistance. Finally, vaccines offer protection from the use of antibiotics to treat secondary bacterial infections; and from their inappropriate use for viral illnesses, which may present with similar symptoms.
3. Evidence of vaccines’ impact on AMR
WHO’s action framework on AMR emphasises that increasing vaccine uptake, particularly in countries with a high disease burden, contributes not only to preventing infection, but also limits the need for treatment and inappropriate use of antimicrobials, thereby reducing the pressure for selecting resistant phenotypes and preserving the efficacy of antimicrobials.14
Research conducted by the One Health Trust into the value of vaccines to mitigate AMR15 found that:
- In Indonesia, reaching 85% pneumococcal conjugate vaccine (PCV) coverage over two years, followed by 99% coverage over three years, could potentially avert antibiotic treatment failures by up to 13.8%.
- Increased PCV coverage has averted approximately 718,100 treatment failures, resulting in a 27.8% reduction in AMR-related deaths between 2011 to 2017.
- A modelling study in 73 countries supported by Gavi, the Vaccine Alliance suggests that 21.2 million cases of multi-drug resistant typhoid fever, 826,000 deaths, and 44.4 million disability-adjusted life years (DALYs) could be averted in children over a ten-year period following the introduction of the typhoid conjugate vaccine (TCV) with a catch-up campaign for children aged up to 15 years.
- In Pakistan, a country dealing with rising levels of extensively drug-resistant (XDR) typhoid cases, a census survey cohort study shows that TCV is over 90% effective in protecting against XDR Salmonella Typhi (S. Typhi) in young children.
- Rotavirus vaccines at 77% coverage in children under two years old in 18 LMICs could avert 13.6 million (31%) episodes of antibiotic-treated diarrhoea annually.
- At 70% coverage, PCV administration in children under two years old across 18 LMICs could avert 23.8 million antibiotic-treated acute respiratory infections annually.
4. Gavi’s contribution to prevent AMR
As of June 2024, Gavi supports vaccines against 20 infectious diseases, some of which are particularly powerful in preventing AMR, such as pneumococcal, typhoid and Haemophilus influenzae type b (Hib). Six vaccines supported by Gavi protect against antimicrobial-resistant diseases by reducing transmission of sensitive and resistant strains, and prevent people becoming ill with difficult-to-treat infections. Many other vaccines included in Gavi’s current portfolio, including those for measles and COVID-19, also contribute to tackling AMR by reducing unnecessary antibiotic use and predisposition to secondary bacterial infections, which then require antibiotic use. In recognition of the contribution that vaccines make to combatting AMR, Gavi’s Vaccine Investment Strategy 2024 now includes ‘impact on AMR’ as an indicator of global health security impact of the vaccines in which Gavi invests.
5. Getting routine immunisation back on track to tackle AMR
As outlined here, the role of vaccines in mitigating AMR is clear and well established. However, vaccines can only meet their full potential for mitigating AMR if they are reaching those who need them, such as the 1 million children aged under five dying from AMR every year.16 Routine immunisation was significantly impacted by the COVID-19 pandemic, as global resources shifted to tackling a global health emergency. Following unprecedented falls in routine immunisation coverage throughout the pandemic, signs of recovery became evident in 2022. The WHO/UNICEF Estimates of National Immunization Coverage (WUENIC) 17 revealed that in 2022:
- The number of children who have not been reached by routine immunisation services – known as ‘zero-dose’ children – reduced from 18.1 million in 2021 to 14.3 million in 2022. This, however, is still below the 2019 pre-pandemic level of 12.9 million zero-dose children.
- Although coverage of the third dose of diphtheria, tetanus and pertussis-containing vaccine (DTP3) recovered to 84% in 2022, this still left 205 million children vulnerable to vaccine-preventable diseases.
- While the proportion of children receiving a first dose of measles-containing vaccine increased from 81% to 83% in 2022, this is still below the 2019 level of 86% and means that 21.9 million children missed their routine first dose of measles vaccine.
Despite signs of recovery, the decrease in immunisation levels during the COVID-19 pandemic has contributed to rising outbreaks of measles, diphtheria, polio and yellow fever, with over 25 million children missing out on at least one vaccine in 2021. As a result, in 2023, WHO, UNICEF, Gavi, the Bill & Melinda Gates Foundation and IA2030 came together with global and national health partners to launch "The Big Catch-up”. This effort aims to reverse the declines in childhood vaccination recorded in over 100 countries since the COVID-19 pandemic, and to lift vaccination levels among children up to at least pre-pandemic levels. Success in achieving The Big Catch-up will play a key role in helping mitigate AMR in the long term.
It is also important to recognise that vaccines are not equitably accessible and available. WUENIC data, for example, shows worldwide coverage of rotavirus vaccine in children is approximately 51%, with significant variation between regions (as low as 29% in WHO’s South-East Asia Region)18 – demonstrating the critical gaps in vaccine access and coverage.
That is why Gavi is focusing on equity and reaching zero-dose children. Every time we reach an unimmunised child, not only do they, their parents and their community gain access to better primary health care, but also we have the opportunity to develop systems and tools for improved resistance surveillance and antimicrobial stewardship. This is why the upcoming high-level meeting on AMR must address the benefits of vaccination for preventing and mitigating AMR.
Conclusions and recommendations
Antimicrobial resistance continues to be one of the greatest public health challenges facing the world, with AMR contributing to 5 million deaths per year, 1 million of which are among children under five years of age.19
While acknowledging the urgency of increased access to new and existing antibiotics, alongside strengthened stewardship of antibiotics, increased investment in and delivery of routine immunisation services can have a significant impact on slowing the progression of AMR.
The high-level meeting on AMR in September 2024 presents a crucial opportunity to highlight the contributions vaccines and immunisation can make towards tackling the global AMR challenge.
Gavi, the Vaccine Alliance urges Member States, the international health community, civil society, private sector and academia to recognise the power of vaccines for preventing AMR and to ensure that this crucial tool is fully incorporated into a comprehensive package of interventions to address the AMR emergency.
More specifically, we make the following public policy recommendations:
Recommendations for governments:
- Integrate immunisation into national AMR action plans and their implementation, in recognition of the critical preventative role they play in tackling AMR.
- Ensure alignment between national AMR action plans and national immunisation strategies to maximise the potential benefits of immunisation on mitigating AMR.
- Strengthen AMR surveillance systems to generate more accurate data on AMR and the contributory factors to AMR, including the preventive role of immunisation.
- Scale up international funding for routine immunisation and reaching zero-dose children, including through The Big Catch-up, to mitigate the long-term impact of missed immunisation on AMR.
- Ensure that vaccines and their crucial preventive role are included in the outcomes of the high-level meeting on AMR.
Recommendations for the international health community:
- Increase awareness of the linkages between immunisation and AMR, clearly demonstrating the preventive effect of immunisation on AMR.
- Invest in research and development to identify more clearly the contribution that immunisation makes to preventing and mitigating AMR.
- Support the strengthening of national AMR surveillance systems, as part of national health surveillance systems, to better identify the contribution vaccines make to preventing and mitigating AMR.
- Promote the inclusion of immunisation in the lead up to, and during, the high-level meeting on AMR.
Recommendations for civil society partners:
- Consider sustaining and scaling up community engagement on immunisation, including identifying and reaching missed communities, and zero-dose and under-immunised children.
- Consider advocating for the inclusion of immunisation as an important contributor to preventing and mitigating AMR in the outcomes of the high-level meeting on AMR.
Recommendations for academia:
- Expand research to strengthen the evidence base on preventive effect of immunisation on AMR, including studies with negative results, which are just as important for contextualising and understanding as are studies with positive results.
- Commit to translating into multiple languages the knowledge gained from research studies and from outside academia to ensure accessibility to policymakers.
References
- World Health Organization, Antimicrobial resistance Fact Sheet: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- Ibid.
- Antimicrobial Resistance Collaborators.(2022) Global Burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022; 399: 629–55 doi: https://doi.org/10.1016/S0140-6736(21)02724-0
- Jonas, Olga B et al. Drug-resistant infections: a threat to our economic future (Vol. 2) : final report (English). HNP/Agriculture Global Antimicrobial Resistance Initiative Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/323311493396993758/final-report
- Comprehensive Review of the WHO Global Action Plan on Antimicrobial Resistance. WHO Evaluation Office. September 2021: https://www.who.int/publications/m/item/comprehensive-review-of-the-who-global-action-plan-on-antimicrobial-resistance-evaluation-brief-september-2021
- Antimicrobial Resistance Collaborators. (2022), ibid.
- An analysis of existing national action plans for antimicrobial resistance—gaps and opportunities in strategies optimising antibiotic use in human populations. Charani, E. Mendelson, M. Pallet, SJC. et al. Lancet Global Health. 2023; 11:e466-74 doi: https://doi.org/10.1016/ S2214-109X(23)00019-0
- Immunization Agenda 2030, A global strategy to leave no one behind: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030
- Leveraging Vaccines to Reduce Antibiotic Use and Prevent Antimicrobial Resistance: An Action Framework: World Health; 2020. Licence: CC BY-NC-SA 3.0 IGO, https://www.who.int/publications/m/item/leveraging-vaccines-to-reduce-antibiotic-use-and-prevent-antimicrobial-resistance
- WHO EB154/CONF//7, 23 January 2024. Antimicrobial resistance: accelerating national and global responses. Draft decision proposed by Australia, China, Ecuador, Egypt, the European Union and its 27 Member States, Japan, Mexico, Norway, Oman, Qatar, Saudi Arabia, South Africa, Switzerland, Thailand, United Kingdom of Great Britain and Northern Ireland and United States of America: https://apps.who.int/gb/ebwha/pdf_files/EB154/B154_CONF7-en.pdf
- O’Neill, J. Vaccines and Alternative Approaches: Reducing Our Dependence on Antimicrobials. The Review on Antimicrobial Resistance, Chaired by Jim O’Neill and published by the Wellcome Trust and HM Government, 2016: https://amr-review.org/sites/default/files/Vaccines%20and%20alternatives_v4_LR.pdf
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. The Review on Antimicrobial Resistance, published by the Wellcome Trust and HM Government, 2014: https://wellcomecollection.org/works/rdpck35v
- Herd immunity can be defined as “the reduction of infection or disease in the unimmunised segment as a result of immunising a proportion of the population”. See John TJ, Samuel R. Herd immunity and herd effect: new insights and definitions. Eur J Epidemiol. 2000;16(7):601-6. doi: 10.1023/a:1007626510002. PMID: 11078115: https://pubmed.ncbi.nlm.nih.gov/11078115/
- Leveraging Vaccines to Reduce Antibiotic Use and Prevent Antimicrobial Resistance, ibid.
- Erta Kalanxhi, Nicole Roberts, Lucy Miller, Felix Bahati, and Ramanan Laxminarayan (2023) The Value of Vaccines to Mitigate Antimicrobial Resistance – Evidence from Low- and Middle-Income Countries. Washington, DC: One Health Trust.
- Antimicrobial Resistance Collaborators.(2022) Global Burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022; 399: 629–55. doi: https://doi.org/10.1016/S0140-6736(21)02724-0
- Progress and Challenges with Achieving Universal Immunization Coverage: 2022 WHO/UNICEF Estimates of National Immunization Coverage. Estimates as of July 2, 2023. WHO/UNICEF: https://www.who.int/publications/m/item/progress-and-challenges
- WHO/UNICEF Estimates of National Immunisation Coverage, data dashboard, https://immunizationdata.who.int/, accessed on 5th May 2024.
- Antimicrobial Resistance Collaborators. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet; 399(10325): P629-655. DOI: https://doi.org/10.1016/S0140-6736(21)02724-0