Vaccine profiles: Diphtheria
Before immunisation for diphtheria became routine, it was a major killer of children and adults worldwide. High vaccine coverage is essential to keep that threat at bay.
- 19 October 2021
- 7 min read
- by Maya Prabhu

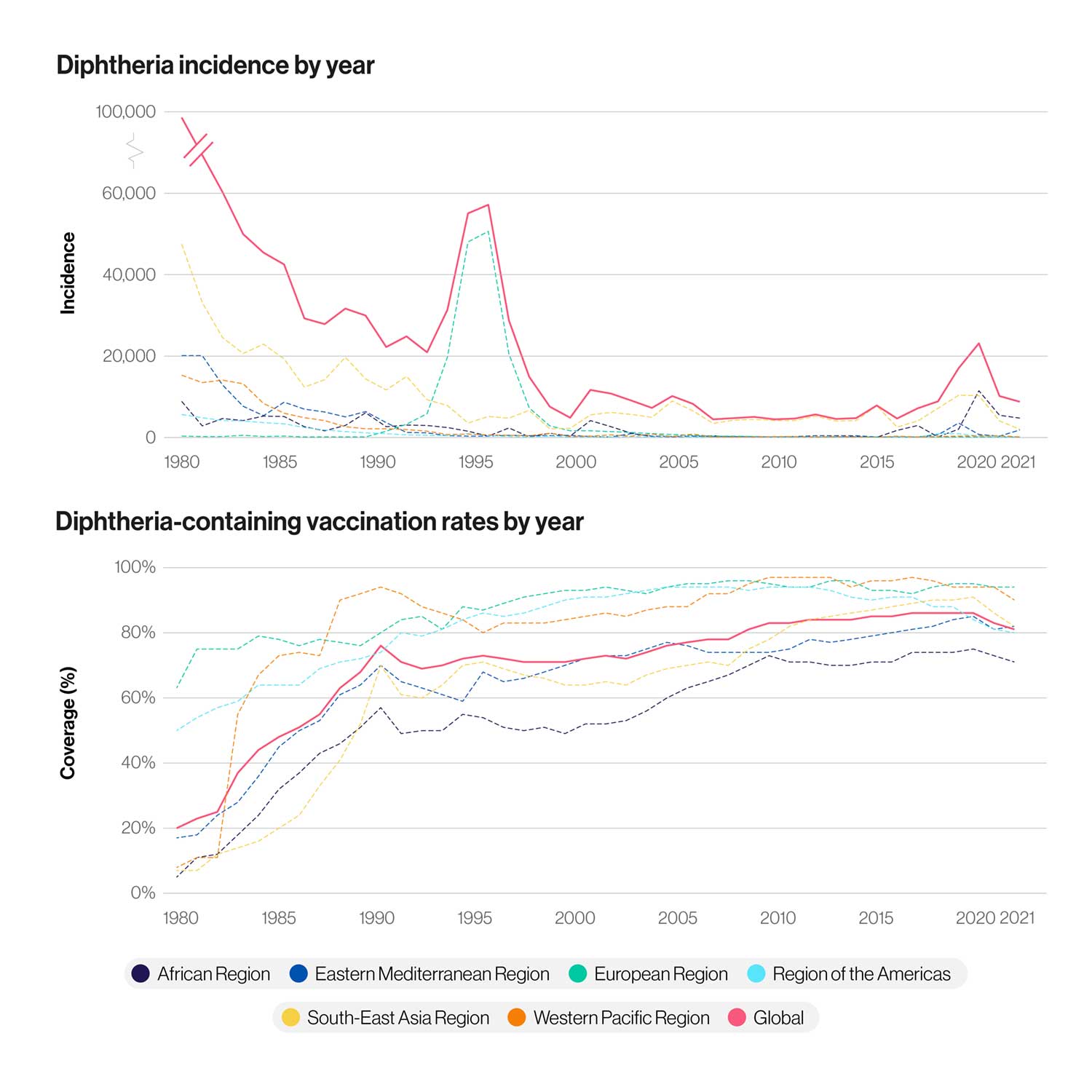
The calamity started small. In 1990, a few paramilitary recruits from southern Russia arrived in Moscow, carrying the causative bacterium in their lungs. The outbreak smouldered for a while among the city’s most vulnerable inhabitants: homeless people, drug and alcohol addicts. But by 1992, diphtheria was making international headlines, with 4,000 Russians reported sick. The following year brought 15,000 more cases.
“We mustn’t take our eye off the ball with diphtheria, otherwise we risk it becoming a major global threat again, potentially in a modified, better adapted, form.”
“Many doctors have forgotten what diphtheria is, and how to treat it,” Moscow’s chief epidemiologist Igor Andreyev told reporters in February 1993, as the deadly outbreak gathered pace. Childhood immunisation against diphtheria had been routine in the Soviet Union since the 1960s; by the mid 1970s, there were fewer than 200 cases a year across the entire country. For many physicians, Andreyev explained, diphtheria was now theoretical – a page in a medical textbook.
Today, diphtheria is largely unheard of in western countries, though it continues to cause sporadic infections or outbreaks in unvaccinated and partially-vaccinated communities worldwide. Yet, the number of diphtheria cases reported globally is increasing, with 2018 showing the highest incidence in 22 years. There’s also evidence that the bacterium that causes it is evolving resistance to a number of classes of antibiotics. Without high vaccine coverage, diphtheria risks becoming a major global threat once more.
Tissue-killing toxin
Diphtheria is an infection of Corynebacterium diphtheriae, a bacterium which can release a tissue-killing exotoxin. Usually transmitted person-to-person via exhaled droplets, diphtheria remains contagious for up to four weeks after infection. The modern name for the disease derives from the Greek for “hide” or “leather”, a reference to the “pseudomembrane” of grey, dead tissue that builds up in the part of the throat behind the mouth and nasal cavity. This can result in a swollen “bull neck” and, in the most severe cases, the toxin can damage the heart, kidneys, and nerves.
The most dangerous form of the disease affects the respiratory system, causing a build-up of dead tissue that obstructs breathing.
Even with proper medical care, one in ten patients with respiratory diphtheria is expected to die; without treatment, case fatality rises to 50%. A less risky form of the disease affects the skin, causing ulcers, but rarely death.
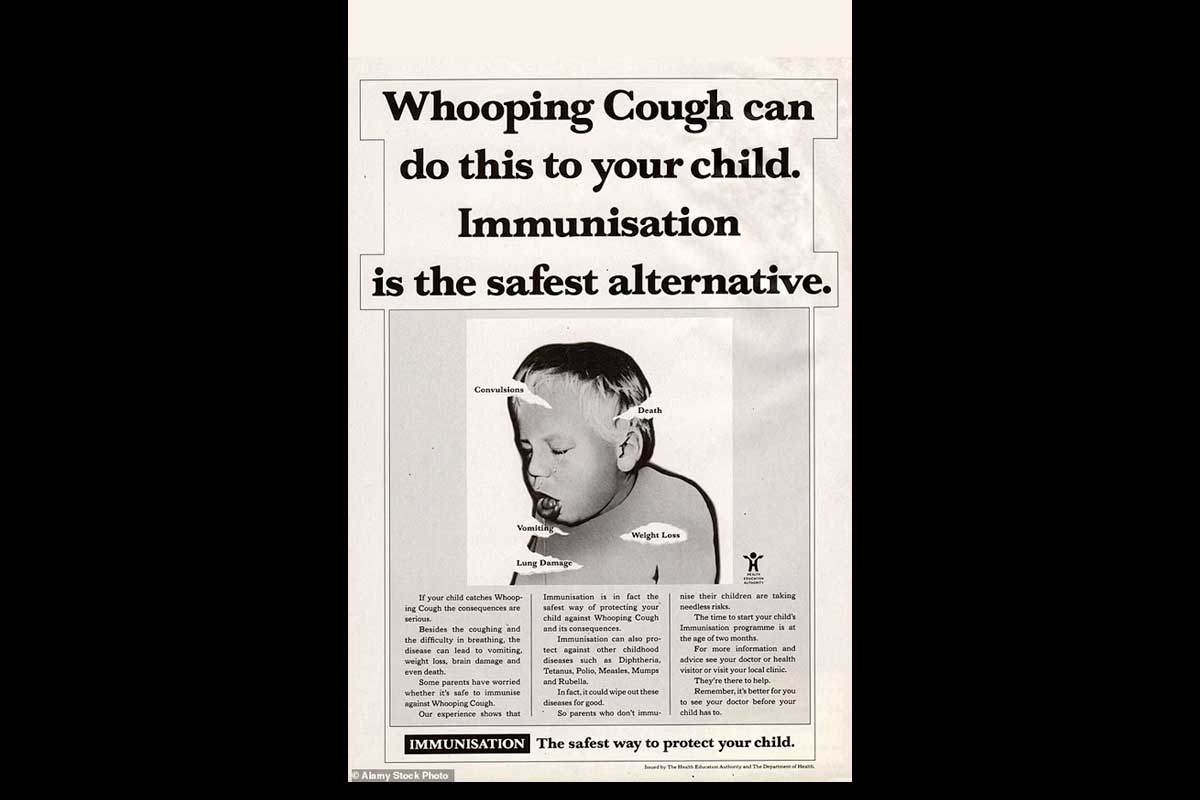
Before widespread vaccination, diphtheria was a major killer of children in the West. Epidemics could be brutal, epochal even: In Spain, the year 1614 was dubbed “El Año de los Garotillos” – the year of strangulations. In one New Hampshire town in 1735, almost a third of children aged under 10 succumbed.
Have you read?
For years, the best treatment was tracheotomy: slicing open the windpipe and inserting a tube to assist breathing. In 1890, scientists discovered how to produce an antibody that counteracted the toxin, by inoculating animals with heat-treated diphtheria toxin, and then purifying this “antitoxin” from their blood. Alongside antibiotics, antitoxin continues to be indicated for the treatment of diphtheria today.
Vaccine development
In 1907, German physiologist Emil von Behring published a paper demonstrating that a carefully calibrated blend of diphtheria toxin and antitoxin could function as a human vaccine. The design was intuitive: the toxin elicited an immune response, and the antitoxin kept the patient safe from full-blown disease. But there was room for improvement. In 1923, two scientists working independently – Gaston Ramon at the Pasteur Institute in Paris, and Alexander Thomas Glenny at the Wellcome Research Laboratories in London, both developed an inactivated version of the toxin called diphtheria toxoid. It was found to be safer and still capable of triggering an immune response.
The mass roll-out of the diphtheria vaccine in Europe, North America, Australia and Japan began in the 1940s and ’50s. The effects were dramatic: In England and Wales, for example, where the disease was endemic, the case-count in 1934 was nearly 100,000. Mass immunisation was introduced in 1942. By 1957, there were only 37 cases.
1974 marked the inauguration of the WHO’s Expanded Programme on Immunization. That year, only 5% of infants in developing countries qualified as “covered” – having received three primary doses of diphtheria toxoid. By 1992, that proportion had soared to 79%.
Lowered guard
However, as the Russian outbreak showed, continued high immunisation coverage remained essential to keeping diphtheria under control. Although childhood immunisation against diphtheria had been routine since the 1960s, the population was gradually becoming more vulnerable. Shifts in the vaccination schedule had widened the gaps between childhood booster shots, and children were increasingly being prescribed lower-antigen, adult-formulation jabs. As the USSR began to splinter, trust in institutional authority dipped, and anti-vaccine campaigners found freshly receptive audiences. According to WHO data, in 1991, just 47% of Russian babies were immunised against diphtheria.
Meanwhile, the immunity of those adults who had once been fully protected was starting to wear off. With a vulnerable population encountering the population-scale upheaval that attended the implosion of the USSR, the epidemic was, as one 1995 Science article claimed, “an accident waiting to happen”.
Before its end in 1996-97, the diphtheria epidemic had spread to all of the ex-Soviet states, infecting more than 140,000 people cumulatively. Sparks of contagion also landed elsewhere: Turkey saw nearly 50 diphtheria patients. Three cases from Russia were exported to Finland, infecting one other person, although here, as in most of Europe, the ramparts of herd immunity resulting from widespread immunisation held.
Caught with its defences down, Russia ramped up vaccine production, immunising nearly 70 million adults between January 1993 and December 1995. In 1994, the childhood vaccination schedule was also amended to plug the gaps, and by 1995, 90% of children had been covered. By 1996, the tide of disease was turning, though across the region, 4,000 lives had been lost.
Combined protection
The diphtheria vaccines we use today are toxoid vaccines – similar, at root, to the Ramon and Glenny innovation. They have been improved with the addition of efficacy-boosting substances called adjuvants, and are commonly packaged with tetanus and pertussis vaccines in the three-in-one DTP jab, considered a core building block of global childhood immunisation programmes, or as part of the five-in-one (DTP-Hib-hepB) pentavalent shot.
This diphtheria-toxoid inclusive DTP vaccine had a global coverage rate of 85% in 2019 – referring to individuals who had received all three primary doses. In July 2020, the WHO and UNICEF warned that the impacts of the COVID-19 crisis on routine immunisation could trigger a decline in DTP3 coverage for the first time in 28 years.
Continued threat
As devastating recent outbreaks have shown, diphtheria remains a cause for alarm, particularly in fragile settings where routine immunisation is interrupted.
In 2017-2018, Cox’s Bazar in Bangladesh – a densely-packed settlement of Rohingya people fleeing persecution in Myanmar – became the site of more than 8,000 reported diphtheria infections and 44 deaths. Yemen, at war since 2014, saw 2,203 “probable diphtheria cases” between October 2017 and August 2018, with 116 deaths.
However, unvaccinated individuals remain at risk anywhere, as the 2015 death of a boy in Spain proved. That risk is only increasing: a 2021 study published in Nature found that C. diphtheria is developing resistance to certain classes of antibiotics. While the paper found no evidence that the vaccine is becoming ineffective, the study authors urge caution. Dr Ankur Mutreja from CITIID, who led the study, said: “It’s more important than ever that we understand how diphtheria is evolving and spreading.” He added, “We mustn’t take our eye off the ball with diphtheria, otherwise we risk it becoming a major global threat again, potentially in a modified, better adapted, form.”