Climate and health crises are converging: we need to tackle them together
As leaders across Africa gather on 4 September in Nairobi to assess continent-wide progress and propose ambitious plans to address climate change, we can only commend this initiative and share their goals to protect the planet and promote the overall health and wellbeing of millions of Africans.
- 4 September 2023
- 5 min read
- by Pascal Barollier

Africa's contribution to the drivers of climate change has been negligible, but its impact on the continent has been disproportionately high. According to the African Union (AU), the death rate from climate change is 60 to 80% higher in Africa than it is in the next most vulnerable region (Southeast Asia). This is largely because many African economies have limited ability to adapt to the impacts of climate change.
Building a vibrant African vaccine manufacturing industry requires capital investment (public and private), technology and knowledge transfer. It also requires business strategies that align production capacities with the expected vaccine demand.
Climate and human health are inextricably linked. As the planet warms, one critical way to adapt is by shoring up our defences against vaccine preventable diseases that are inevitably evolving and spreading wider than before. Immunisation can help African countries combat the effects of climate change by creating resilient health systems and healthier populations that are able to withstand our warming planet. In this sense, Gavi's mission and Africa's priorities are fundamentally aligned: working in tandem to predict, prevent and manage the impact of climate change on the continent.
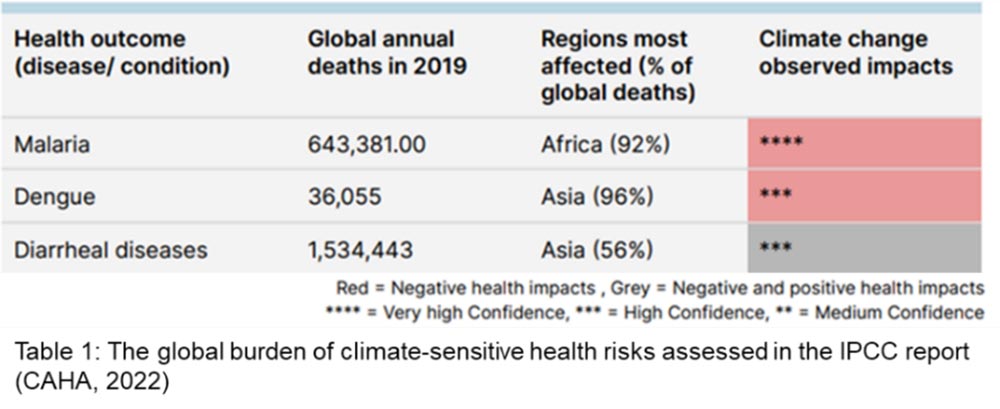
Reducing vulnerability to climate-driven diseases
Warmer temperatures and higher rainfall are increasing the habitat suitability for mosquitoes and driving the transmission of vector-borne diseases such as dengue fever, malaria and yellow fever. By 2050, climate change could increase yellow fever deaths in Africa by 25%, and by 2100, an additional 2.25 billion people globally are likely to be at risk of dengue.
Spikes in flood-related disasters are also increasing the occurrence of diarrhoeal and waterborne diseases, such as rotavirus. Models predict the relative risk of diarrhoeal disease could increase by 8–11% from 2010–2039 due to climate change. The majority of the additional deaths due to diarrhoeal diseases are expected to occur in Africa.
This is where vaccine stockpiles come in – both as a measure of last resort when a disease outbreak occurs as well as preemptive measure for at-risk populations susceptible to climate-sensitive diseases.
To date, Gavi, the Vaccine Alliance has helped 17 countries in Africa introduce the yellow fever vaccine into their routine immunisation programmes. In addition, Gavi-supported yellow fever vaccine campaigns in 14 African countries have protected over 133 million people. Furthermore, over 62 million doses from the emergency stockpile have reached Gavi-supported countries experiencing yellow fever outbreaks.
Have you read?
There's no doubt that yellow fever vaccine is highly effective: a single dose leads to long-term, possibly even lifelong, immunity in 99% of people vaccinated. Yet, despite Africa's vulnerability to sudden climate change and disease outbreaks, African nations do not have yet the benefit of domestic or regional vaccine manufacturing capacity or an independent continental strategic stockpile. As the figure below demonstrates, the continent is almost absent from the manufacturing landscape, accounting for approximately 0.2% of global supply.
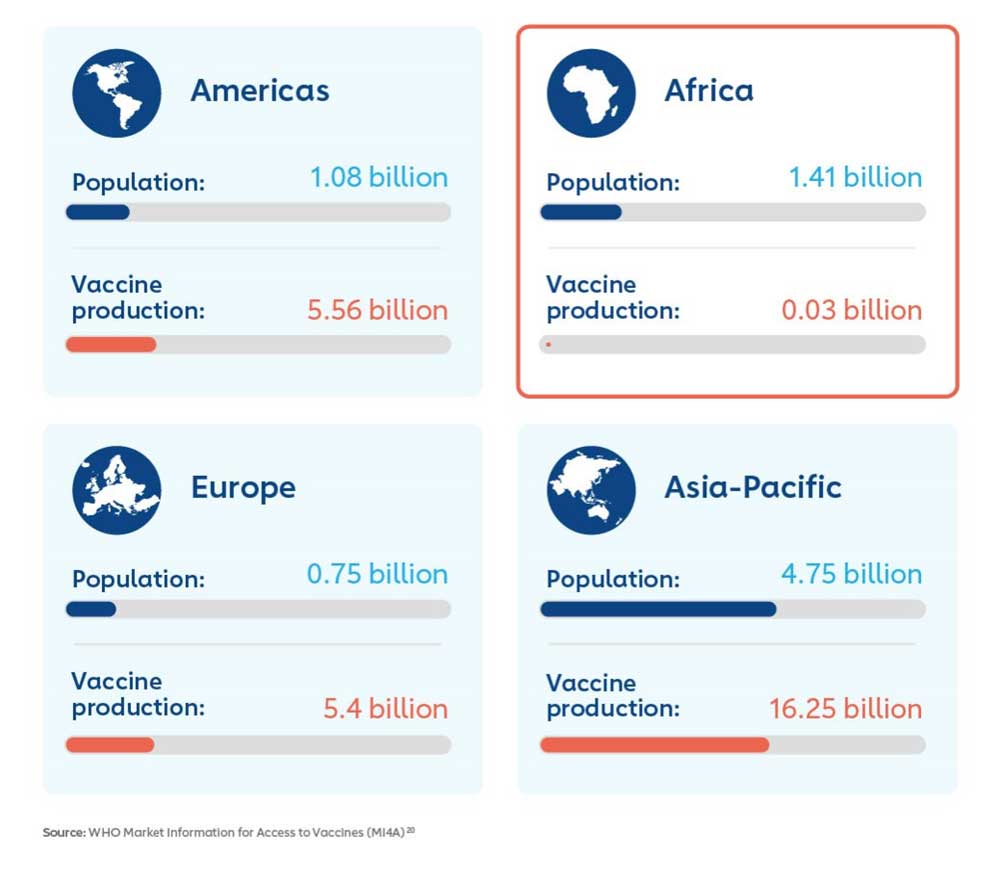
Building a vibrant African vaccine manufacturing industry requires capital investment (public and private), technology and knowledge transfer. It also requires business strategies that align production capacities with the expected vaccine demand. In parallel, quality assurance, stringent and independent regulatory review, resilient supply chains, and other supportive systems need to be in place. These priorities are at the centre of the goal and strategy of the Partnerships for African Vaccine Manufacturing (PAVM) established by the AU under Africa CDC.
The continent is employing a bold new homegrown approach to build the infrastructure that can support long-term growth, move up the manufacturing and industrial value chain, while also delivering climate resilience.
In support of this, and to help drive African-led solutions that leverage the private sector, global health partners are looking at ways to incentivise capital investment in sustainable facilities that directly meet public health needs. A benefit could be to direct manufacturers towards production in the most viable markets, helping to secure accelerated, competitive entry of new manufacturers where there is an unmet market need.
Being ready for crises before they occur
The African Union Climate Change and Resilient Development Strategy and Action Plan notes that if a small proportion of the resources that are channelled into disaster relief and recovery is invested into effective early warning, preparedness and resilience-building, the negative impacts and reconstruction costs will be greatly reduced. The establishment of early detection and warning systems, resilient health systems, and disease surveillance, is considered a critical aspect of climate adaptation. By supporting countries' investments in systems for vaccine-preventable disease monitoring and detection, such as the modernisation and scale-up of electronic health management information systems (e-HMIS) we can strengthen the resilience of routine immunisation, ease climate-related shocks and help African countries manage climate risks effectively and proactively.
Solidarity to save lives
Finally, as the effects of climate change are felt across multiple regions and sectors, it's important for us to transcend silos. This includes breaking barriers across sectors to formulate and implement health and climate change plans. This will enable a comprehensive health response to climate change, which enhances population resilience to climate risks, and supports health-promoting climate change mitigation policies.
But above all, we need solidarity and coordination among countries, among international organisations and among the activists and civil society groups working to face down these threats.
Website
This article was originally published on Pascal's LinkedIn on 1 September 2023.