Fighting antimicrobial resistance in the world’s biggest consumer of antibiotics
India been called both the 'pharmacy of the world' and the 'epicentre of AMR'. TV Padma looks at drug resistance trends in the world’s most populous nation.
- 20 September 2024
- 6 min read
- by T V Padma

The 79th session of the United Nations General Assembly (UNGA) is set to convene the second-ever High-Level Meeting on the rise of antimicrobial resistance (AMR), a danger the World Health Organization (WHO) has termed “one of the top global public health and development threats”.
Indeed, it’s estimated that already in 2019, bacterial AMR was directly responsible for 1.27 million deaths worldwide, and a contributing factor in 4.95 million deaths. Resistance continues to spread.
The major driver for the increasing invulnerability of pathogens to antimicrobial drugs is the misuse and overuse of antimicrobials in humans, animals and plants. That’s principally in terms of the way they are consumed – but production norms are also a danger zone.
In India, more than half of antibiotics prescribed to patients are prescribed for preventing possible infections, rather than treating existing ones.
The WHO this month released a guidance document for wastewater and solid waste management in the manufacturing of antibiotics to provide “an impartial scientific basis for regulators, procurers, inspectors and the industry themselves to include robust antibiotic pollution control in their standards”.
One market in which the document will hope to find a ready audience is India. Often called the “pharmacy of the world” for its large-scale production of medicines, India is also the world’s biggest consumer of antibiotics for human health in absolute, though not per capita, terms. It’s not coincidental that the country has also been labelled an “epicentre of AMR”.
AMR in India
The 2023 annual report of the Indian Council of Medical Research (ICMR) AMR surveillance network looked at antibiotics that are commonly used to treat upper respiratory tract infections, fevers, diarrhoea, pneumonia, sepsis and other bloodstream infections in the country.
It found that Escherichia coli, which causes stomach infections, was the most commonly isolated drug-resistant pathogen, followed by Klebsiella pneumoniae, which can cause a range of infections from pneumonias to urinary tract infections; Acinetobacter baumannii, which is increasingly causing hospital-acquired infections, Pseudomonas aeruginosa, notorious for causing infections after surgery; and Staphylococcus aureus, responsible for skin infections and sepsis, among other health problems. E coli and K. pneumoniae showed increasing resistance to most drugs.
Yet consumption is far from cautious. In India, more than half of antibiotics prescribed to patients are prescribed for preventing possible infections, rather than treating existing ones, according to a 2021–22 survey on antibiotic use in India conducted by the ICMR’s National Centre for Disease Control (NCDC). Fifty-seven percent of all the antibiotics being prescribed to patients taking part in the survey fell under the WHO’s “watch group” of drugs that are at higher risk of developing resistance in their target pathogens.
In July this year, a study by Tavpritesh Sethi of the Indraprastha Institute of Information Technology and colleagues, published in the Lancet Regional Health, found high, and rising, resistance rates to critically important antimicrobials like Imipenem, an antibiotic used to fight Acinetobacter, Klebsiella and E. coli infections.
The study was a retrospective analysis of data spanning the six years from 2017 to 2022. The researchers used statistical and machine learning techniques to estimate trends in resistance and bloodstream infections (BSIs).
Vaccines for combatting bacterial pathogens offer hope for lowering medical costs and reducing poverty, say scientists
They found that resistance trends varied by region. Drug resistant E. coli BSIs were found to be more prevalent in isolates from southern India, while resistant Staphylococcus was more common in the north.
AMR Acinetobacter showed higher prevalence in the central and north-east zones. In contrast, Klebsiella, P. aeruginosa, and Enterococcus showed a more uniform distribution across the regions . A high rate of multi-drug resistance was observed in Klebsiella, Acinetobacter, and Staphylococcus isolates.
Can vaccines help?
The potential impact of vaccination in reducing antibiotic use in low- and middle-income countries (LMICs) is immense, with vaccines for combating bacterial infections offering hope for lowering medical costs and ultimately reducing poverty, India-based scientists specialising in AMR told VaccinesWork.
That said, a vaccination-centred AMR strategy does present logistical challenges - not least because certain infections don’t have vaccines that can block them. Some scientists have argued for the positioning of AMR as a global priority, to mobilise the kind of emergency action that propelled the record-paced development of COVID-19 vaccines.
Studies have shown significant reductions in antibiotic prescriptions following vaccine programmes, such as a 64% decrease in Ontario, Canada, and up to 88% in paediatric cohorts in Italy, Japan and Pakistan.
But beyond blocking specific pathogens from taking hold, and thereby doing away with the need to deploy antimicrobials to beat them back, vaccines also play a crucial role in combatting AMR by reducing the incidence of viral infections that can predispose individuals to bacterial colonisation.
For instance, influenza can deplete immune cells, increasing the risk of bacterial co-infections. But vaccination helps lower viral loads and infection duration, minimising the window of vulnerability to bacterial invasion. The same pattern is true for measles, a virus that attacks immune cells directly. The majority of children who die with measles, die from bacterial co-infections.
Studies have shown significant reductions in antibiotic prescriptions following vaccine programmes, such as a 64% decrease in Ontario, Canada, and up to 88% in paediatric cohorts in Italy, Japan and Pakistan.
Vaccination against mild chickenpox infections could also drastically cut antibiotic-related costs. Additionally, flu vaccines in countries like Senegal and South Africa could prevent 390 antibiotic prescriptions per 100,000 people annually, highlighting their potential in reducing antibiotic misuse and combating AMR.
While there is an urgent need for efficacious new antibiotics to manage bacterial infections, the use of vaccines can extend the longevity of current as well as future antimicrobials.
Promising pipeline
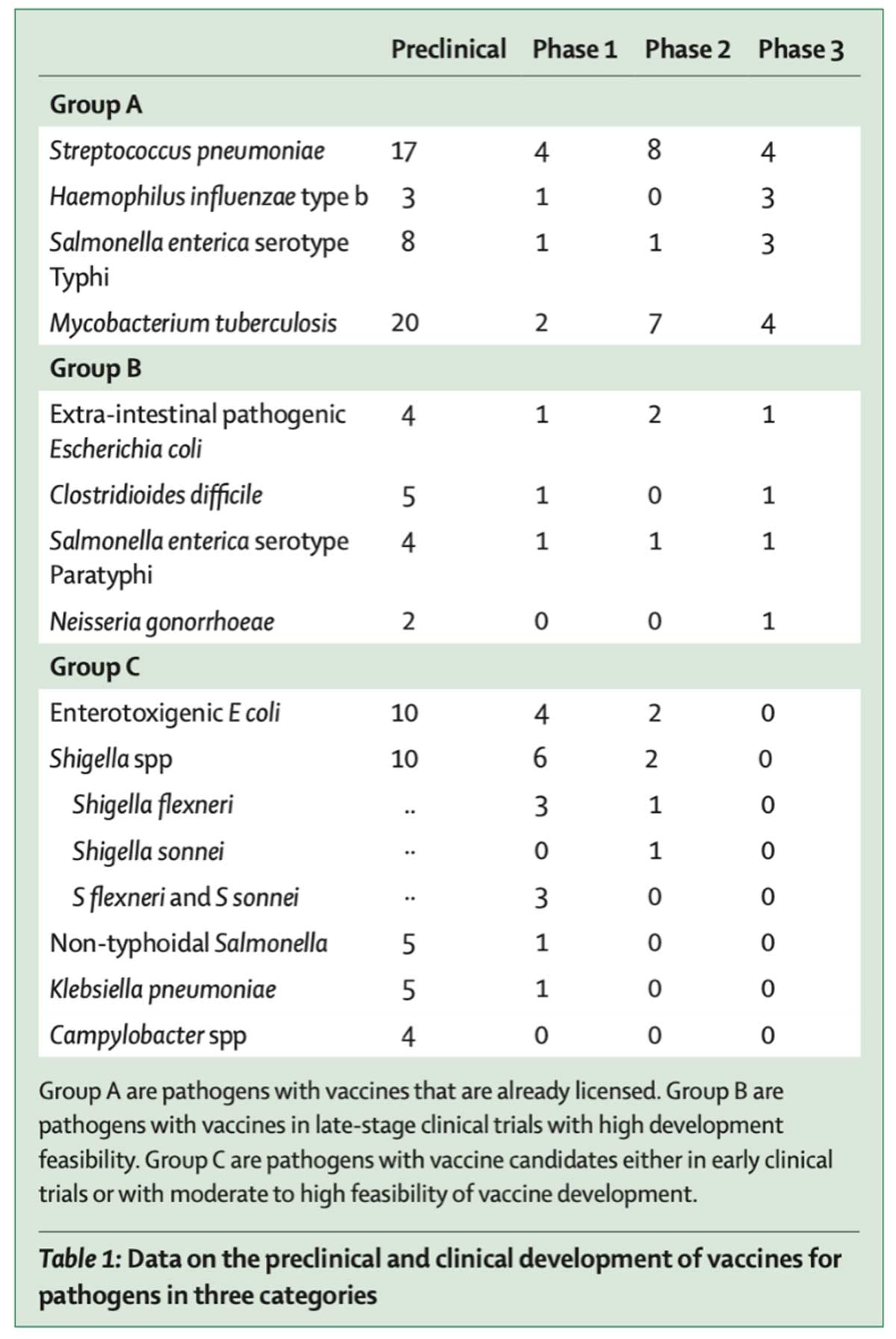
The WHO identified and reclassified high-priority pathogens into three groups, according to the feasibility of vaccine development against them:
i. Pipeline Feasibility Group A (very high): Pathogens for which licensed vaccines already exist. The focus is to increase the coverage of authorised vaccines.
ii. Pipeline Feasibility Group B (high): Priority pathogens for which a vaccine candidate is in late-stage development. The focus is to accelerate their development.
iii. Pipeline Feasibility Group C (moderate): Priority pathogens for which a vaccine candidate is in early clinical trials or understood in expert reviews. The focus is to generate knowledge on the potential for vaccine use and its impact.
Currently, it's clear that vaccines are underutlilised as a critical component of AMR strategy to complement other interventions like stewardship, and the development of new antibiotics -- which are sorely needed for key AMR pathogens like TB, Staphylococcus aureus, Klebsiella pneumoniae, and Gonococci.
To further bolster innovations in addressing AMR, especially in LMICs, there are additional areas of potential breakthroughs and innovation such as rapid diagnostics and point-of-care testing; antimicrobial peptides (AMPs) or small pieces of peptides that inhibit some bacteria, viruses, fungi and pathogens; phage therapy that uses viruses that infect and kill some bacteria; artificial intelligence-driven drug discovery; nanotechnology-based drug delivery systems; and management of the gut microbiome, among others.
These innovative approaches can help tackle AMR from multiple angles – diagnostics, treatment, prevention, and environmental management – addressing what truly is an existential global health challenge.








