HIV progress raises life expectancy in Africa - UN
Successes in treating people with HIV led to life expectancy in Africa rising from 56 to 61 years since 2010.
- 23 July 2024
- 5 min read
- by SciDev.Net

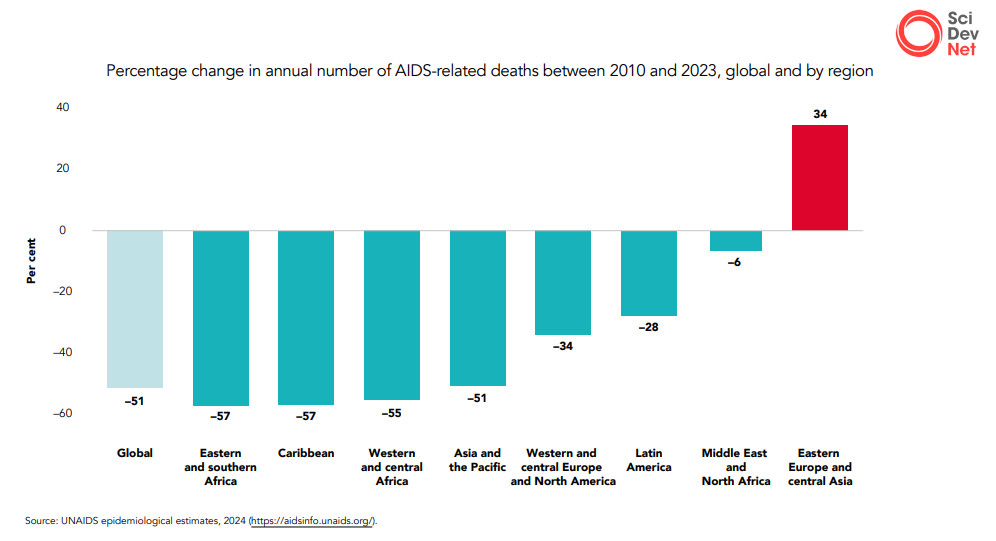
Average life expectancy in Sub-Saharan Africa jumped from 56 years in 2010 to 61 years in 2023 thanks to progress made in the fight against HIV/AIDS, according to a global UN report.
The success stands in contrast to the “hesitant” HIV response elsewhere in the world, amid rising HIV rates in at least 28 countries, according to the analysis published today (22 July) by the Joint United Nations Programme on HIV and AIDS (UNAIDS)
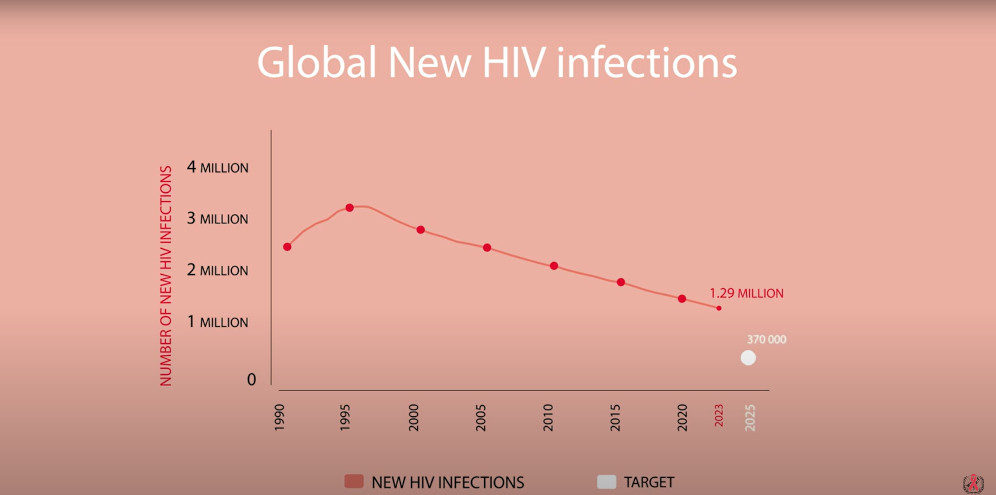
According to the report, around 31 million people were on antiretroviral treatment in 2023, reducing deaths linked to the disease to 630,000, their lowest level globally since the 2004 peak of around two million.
Anne-Claire Guichard, senior policy advisor at UNAIDS and one of the report’s authors, says linked or integrated treatment of TB and HIV for people living with both diseases, prevented around 6.4 million deaths worldwide between 2010 and 2022.
During that time there was a 39 per cent decline in new HIV infections “mainly due to progress in Sub-Saharan Africa”, according to Guichard.
“Between 2010 and 2023, East and Southern Africa saw a 59 per cent reduction and West and Central Africa a 46 per cent reduction in the annual number of people with HIV.”
She notes that nine countries, including seven in Africa, have met the UN’s 95-95-95 treatment goals, which aim to diagnose 95 per cent of all HIV-positive cases, provide antiretroviral therapy (ART) for 95 per cent of those diagnosed, and achieve viral suppression for 95 per cent of those treated. Saudi Arabia, Botswana, Denmark, Eswatini, Kenya, Malawi, Rwanda, Zambia and Zimbabwe have all achieved this.
Globally, of all people living with HIV in 2023, 86 per cent knew their HIV status, 77 per cent had access to treatment and 72 per cent had an undetectable viral load.
For the first time, the number of new infections outside Sub-Saharan Africa surpassed the number of new infections in Sub-Saharan Africa, according to the report.
However, despite this progress, the number of new infections in Sub-Saharan Africa remains high — 640,000 out of the 1.3 million recorded worldwide in 2023. Out of 630,000 people who died from the disease in 2023, 390,000 were from Sub-Saharan Africa, home to 25.9 million of the 39.9 million people living with the disease worldwide.
Eric Delaporte, an infectious diseases doctor and research director at the French National Research Institute for Sustainable Development (IRD), told SciDev.Net: “We must not forget that Africa was by far the most affected continent and for which the challenges were the most important to overcome.”
He highlighted the fact that treatment for HIV/AIDS is a lifelong process, made more difficult as people who are sick with the disease grow old.
“They will be confronted with pathologies linked to age and/or sometimes to the side effects of treatment, and for which there is not necessarily access to free treatment,” said Delaporte.
“It’s yet another new challenge to overcome which shows to what extent efforts must be maintained.”
Stretched resources
The French researcher also blames the effects of the global pandemic, including resources redirected towards COVID-19 and the impact of containment measures, such as disruptions to medical supplies and accessing clinics.
In Africa these challenges were compounded by socio-economic factors such as poverty and humanitarian crises, says Fogué Foguito, executive director of the NGO Positive Generation, which promotes health and human rights in Cameroon.
“We also have environmental factors such as stigma and discrimination, including a legal and legislative environment that does not sufficiently promote the protection and promotion of human rights, particularly among HIV-positive people,” he said.
UNAIDS director Winnie Byanyima, in a foreword to the report, said a widening funding gap, exacerbated by the global debt crisis, was “holding back the HIV response in low- and middle-income countries”.
Funding for HIV dropped by five per cent from 2022 to 2023, and by 7.9 per cent between 2020 and 2023, the report indicates.
“About US$19.8 billion was available in 2023 for HIV programmes in low- and middle-income countries — almost US$9.5 billion less than the amount needed by 2025,” noted Guichard.
Have you read?
Women and children
Among the hardest hit by these shortfalls are children and women, the report suggests. Every week, 4,000 adolescent girls and young women aged 15 to 24 contracted HIV worldwide in 2023. And 3,100 of these infections occurred in Sub-Saharan Africa.
In West and Central Africa, just over a third (35 per cent) of children living with HIV received treatment in 2023, according to Guichard.
“The region is home to 20 per cent of pregnant women living with HIV worldwide, but almost half of them … are not on treatment,” she added.
For Foguito, the HIV burden among children and adolescents is “a moral fault for all of us”.
“Everyone must ask themselves the question of how they can … make their modest contribution to reversing this trend,” he said, adding that real political will has almost never “gone beyond speeches and summits in large hotels or conference centres”.
The report recommends a “sustainable response” which according to Guichard “must be based on data, rely on solid integrated national systems guaranteeing equitable access to services and innovations, and rely on political will, in addition to being fully funded”.
The authors predict that there will still be almost 30 million people living with HIV in 2050, each needing lifelong treatment.
The Global Fund to Fight AIDS, Tuberculosis and Malaria says the report highlights the “urgent need” to accelerate progress in preventing HIV.
“To effectively combat the HIV epidemic, we must break down barriers that hinder access to prevention services, especially for marginalized populations,” said the fund’s executive director, Peter Sands.
He cited as a “promising example of innovation in prevention” the dapivirine vaginal ring, which reduces women’s risk of infection by continually releasing antiretroviral drugs into the vagina.
This article was produced by SciDev.Net’s Sub-Saharan Africa French edition and edited for brevity and clarity.