Is COVID-19 about to take off in Africa?
So far relatively few people in Africa have been infected by the novel coronavirus, with around 215,000 cases and 5,800 deaths in a population of 1.2 billion in the continent. But with lockdowns lifting, will cases soar?
- 17 June 2020
- 5 min read
- by Gavi Staff

Since the start of the pandemic, concerns have been raised by governments and global health stakeholders over the ability of countries to respond to COVID-19. As the crisis escalated, it became evident that even high-income countries were woefully unprepared to respond adequately and prevent the continued transmission of the virus. Shortages of medical supplies and equipment such as diagnostic test kits, ventilators, intensive care unit beds, disinfectant and personal protective equipment for health workers created a global competition among governments.
Within the African continent, these challenges have been exacerbated due to the lack of strong health systems, and limited access to clean water and sanitation, as well as other factors, such as urban density and crowded living conditions. On 14 February 2020, Africa reported its first coronavirus case in Egypt and since then the number of cases has risen, exceeding 215,000 across the continent.
Until now, COVID-19 cases have been increasing in Africa at a steady and, more or less, predictable rate but according to Dr Matshidiso Moeti, the World Health Organization’s (WHO) Regional Director for Africa, this has taken a quick turn. “It took 98 days to reach the first 100,000 cases, and only 18 days to move to 200,000 cases,” she said.
Was it too early to lift lockdown?
Several African governments responded swiftly to the first few COVID-19 cases, implementing lockdowns, enforcing curfews, closing schools and borders, and banning entry of foreign travellers. Nigeria, for example, closed schools after only eight confirmed COVID-19 cases.
However more recently, despite WHO advice, Djibouti, Ghana, Nigeria, and South Africa have decided to ease lockdown restrictions to strike a balance between managing economic losses and keeping coronavirus transmission to a minimum. One key reason for this is that many people across Africa work in the informal economy earning wages for hours worked or services delivered, which means they would not be able to survive for long without work.
However, the lifting of restrictions has had negative consequences; for example, in Ghana, a week after lockdown was lifted, the country recorded 508 new cases, an increase of 50% in just one week.
Similarly, in South Africa, following a robust testing programme, a particularly high number of COVID-19 cases were reported and has seen the rate of increase in the number of cases remain stable since the confinement measures have begun to be relaxed. Regardless of the lockdown situation, WHO urges that countries must remain vigilant and ensure that testing and surveillance systems are effective to enable detection of any spike in cases.
How are Gavi-supported countries in Africa coping with COVID-19?
As of 11 June 2020, 37 of the 40 Gavi-supported countries in Africa have COVID-19 cases in their countries with a total of 77,923 cases and 1,594 deaths across these countries. Gavi’s COVID-19 support to countries includes providing much-needed funding for vital personal protective equipment (PPE), diagnostics and training, with 27 countries in Africa benefitting from this immediate support.
Gavi has seen significant disruptions across all health services but particularly in routine immunisation (RI) – a recent WHO survey reported a 64% partial or complete disruption of routine immunisation at health facilities and a 73% partial or complete disruption of outreach in routine immunisation. “A major cause of this interruption is the lack of access to PPE for health workers. We are targeting this disruption on the African continent by allocating nearly half of our approved reprogrammed health systems strengthening funding towards infection prevention and control, of which ~US$ 19 million has already been used to purchase face masks, gloves and hand sanitizer through UNICEF Supply Division,” said Pascal Bijleveld, Gavi’s Director of Country Support, on how Gavi is supporting the response to this challenge.
Uganda
Uganda has seen a reduction in the numbers of people accessing health services as many believe that the national COVID-19 stay-at-home orders prevent health care facilities from remaining operational for routine services such as immunisation and antenatal care. Though Uganda has shown a renewed commitment to immunisation, doubling funds in the 2019-2020 budget, misinformation and fear have become obstacles in ensuring continuous uptake of routine immunisation services during the pandemic. Furthermore, health workers’ availability was limited for other health services as they were focussed on supporting COVID-19 response and also due to lack of PPE. To combat this, Uganda is already making evidence-based plans for rolling out catch-up immunisation campaigns during the post-COVID-19 period.
Gavi has thus far supported the government of Uganda by approving a US$ 3,120,539 reallocation of existing funds going towards diagnostics test kits and related commodities.
Senegal
Innovation has been at the forefront of Senegal’s COVID-19 response as two types of affordable, rapid COVID-19 tests are in development – one using saliva, the other a drop of blood. These tests will cost less than US$ 1 to produce and will provide a diagnosis within 10–20 minutes. Furthermore, university researchers are creating artificial respirators almost entirely using a 3D printer.
However, routine immunisation services are proving difficult to maintain due to a national state of emergency declared by President Macky Sall from 23 March till the end of June. This state of emergency imposed limits on public transport, a curfew and the closure of schools and universities. Compounded with the rumors and fear around COVID-19, the limited implementation of vaccination outreaches and the stigmatisation of families and communities affected by COVID-19 have inhibited routine immunisation. The lockdown measure of school closures caused a 10% coverage drop in April compared to January for measles-rubella vaccine and 39% for human papillomavirus (HPV) vaccine. In response, the country is working with partners to reinforce the strategy to maintain essential health services including immunisation and to follow-up with children who missed out on routine immunisation services after the COVID-19 pandemic subsides.
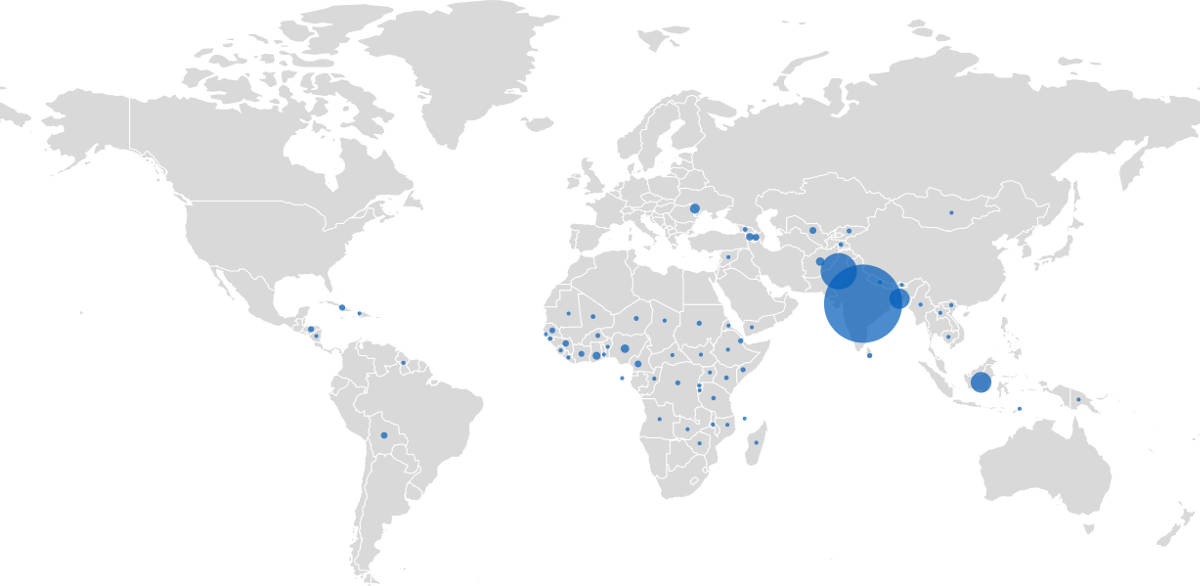
COVID-19 dashboard
Find out about the latest situation in Gavi-supported countries and the rest of the world.