Why bird flu vaccines need urgent R&D
As bird flu has started to show up in mammals, concerns continue that the virus might mutate to spread amongst people. If that happens, we’d need a vaccine, fast – here’s where we are so far.
- 15 February 2023
- 5 min read
- by Priya Joi

Currently, the worst ever outbreak of bird flu is causing mass die-offs in poultry and other birds, and is starting to be seen in animals from otters to dolphins. If the virus evolved to be able to spread easily between people, the concern is it could trigger another major global outbreak.
In general, bird flu doesn’t infect people easily [...] However, the fact that the current global H5N1 bird flu outbreak has caused such large die-offs and has started to spread in small mammals means that some scientists are concerned.
Since the 1918 flu pandemic, there have been three flu pandemics – H2N2 in 1956-7, H3N2 in 1968 and H1N1 in 2009 – and before COVID-19 many scientists were predicting that the next pandemic would be caused by a flu virus. If that happens, vaccines will be critical in preventing the spread, yet while we do have vaccines against two bird flu viruses, they will be difficult to scale up should we need them.
Strains of bird flu causing concern
The influenza viruses that infect birds are influenza A viruses. Five subtypes are known to have caused human infections: H5, H6, H7, H9, and H10 viruses. In particular, A(H5N1) and A(H7N9) viruses have caused the majority of avian influenza virus infections reported in people, with HPAI A(H5N6) and LPAI A(H9N2) viruses also causing human infections in recent years. In 2021, H5N8 infected people for the first time in a poultry farm in Russia.
In general, bird flu doesn’t infect people easily – the virus binds to receptors in the upper airways of birds that are not as common in mammalian upper airways, which means it is much harder for infected mammals to spread it. Those affected tend to have been in close contact with the animals, such as farm workers, and it doesn’t easily spread between people.
However, the fact that the current global H5N1 bird flu outbreak has caused such large die-offs and has started to spread in small mammals means that some scientists are concerned that the virus could evolve to spread more easily among human beings, potentially triggering another pandemic.
Why not just vaccinate birds?
Vaccinating birds against flu is not easy. In 2017, China began mandatory vaccination of poultry against an H7N9 strain that was able to spread to people, thereby stemming the spread of the virus. But this strain affects fewer varieties of birds, unlike H5N1.
Moreover, public health officials are worried that if vaccination isn't carried out properly, the virus could continue circulate at a low level, actually increasing the chance of mutations and spread to people.
Given the potential threat, the US is to test a vaccine that could be given to poultry in a bid to staunch the spread of the virus.
Have you read?
The chicken and egg problem
Although several H1N1 and H5N1 vaccines have been approved by the US Food and Drug Administration, scaling up could take many months. This is due to the fact that all but one are produced by incubating each dose in an egg (the same way that human flu vaccines are made).
"We haven't yet tried mRNA vaccines with these viruses; we know they work to some degree, but how well they'd work and what level of protection they'd induce is still an open question."
Researchers Ian Barr and Michelle Wille
Inevitably, the process is slow. The live virus is injected into an embryonated chicken egg, and then once the virus has replicated the viral material is collected, inactivated and the antigen purified. This process is too laborious to scale up in an emergency, not to mention the fact that a virus that targets poultry could lead to severe egg shortages, thereby preventing scale-up.
Cell-based vaccine manufacturing technology could be the answer. In this system, viruses are grown in closed systems of large numbers of cells in growth media.
In late 2021, Seqirus received FDA Approval for the first-ever cell-based pandemic influenza vaccine. Scaling-up production of this non-egg-based H5N1 vaccine could result in 150 million doses within six months of the declaration of a pandemic, but this still wouldn't be enough to protect the world.
Stockpiling vaccines for viruses such as influenza is also challenging because the virus is constantly evolving – this is why seasonal flu vaccines are developed anew every year.
Moving to mRNA technology
Vaccines do exist, but these traditional vaccines “do not produce really good, strong immune responses in humans”, researchers Ian Barr and Michelle Wille told Gavi. “We haven’t yet tried mRNA vaccines with these viruses; we know they work to some degree, but how well they’d work and what level of protection they’d induce is still an open question.”
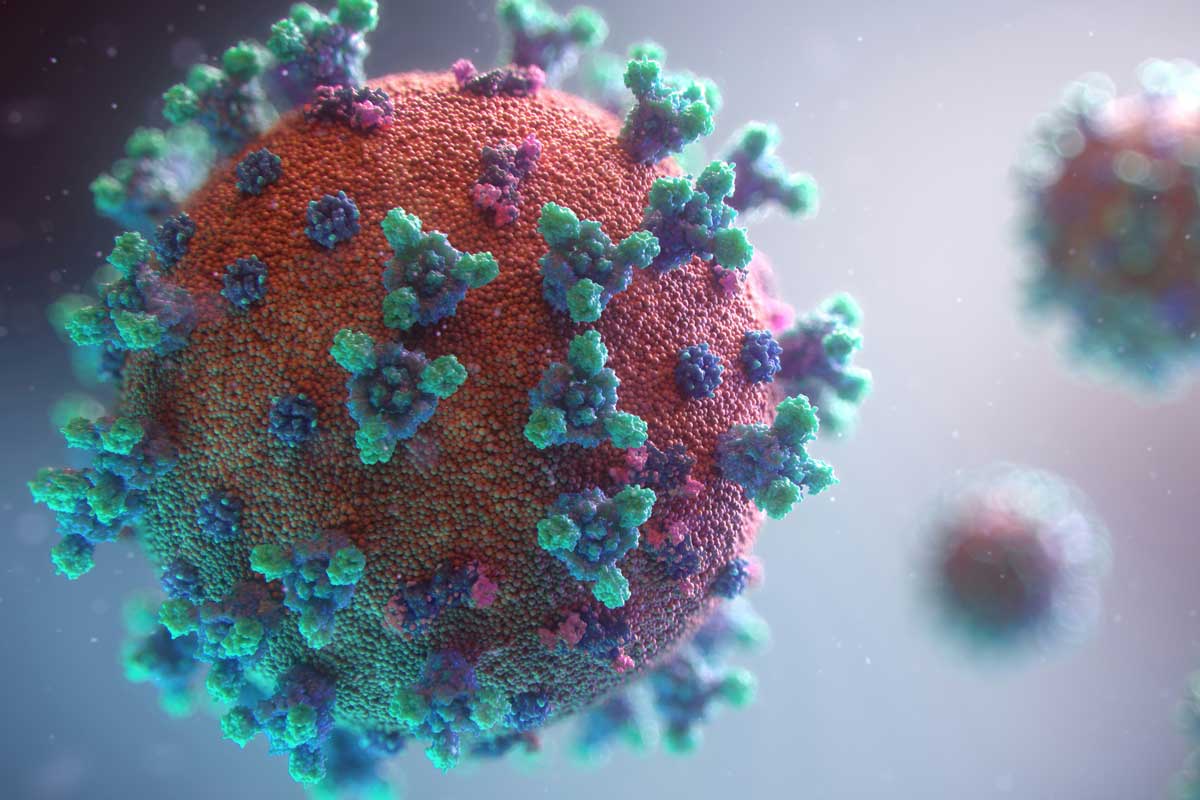
Initial studies seem promising. In November 2022, a paper published in Science showed that a flu shot against all 20 known subtypes of influenza A and B virus protected mice and ferrets against several strains of flu.
The two-dose vaccine uses the same mRNA technology used to make COVID-19 vaccines, except this time it delivered small particles containing the instructions for making the haemagglutinin proteins found on the surface of the influenza virus into cells. The cells start manufacturing these proteins, triggering an immune response.
The real question now is how quickly such vaccines could be scaled up in the event of a pandemic.
More from Priya Joi
Recommended for you