What is contact tracing, how could it reduce the spread of COVID-19, and how could it affect me?
Controlling the pandemic demands a multi-pronged approach with other key methods like contact tracing to help stop the chain of transmission.
- 19 May 2020
- 5 min read
- by Elinore Court

What is contact tracing?
Contact tracing is a process that involves identifying anyone that has been in close contact with someone who has tested positive for an infectious disease. These contacts should then be notified, closely monitored and, in the case of COVID-19, quarantined for 14 days even if they do not display symptoms. The World Health Organization (WHO) then recommends regular follow-ups to “monitor for symptoms and test for signs of infection.”
In order to be effective and rapidly identify potential virus hotspots, anyone that has tested positive must provide a list of their recent activities and people they’ve come into close contact with.
These contacts should then be notified and closely monitored for the duration of the incubation period, which is the length of time between exposure to a virus and the onset of symptoms. The incubation period can vary with different diseases, so while it is typically 14 days for COVID-19, anyone in contact with an Ebola patient should be monitored for symptoms for 21 days.
How has it been effective throughout history?
Contact tracing was also used as a “test, trace and track” method to control Ebola outbreaks across Africa and played a crucial role in the eradication of Smallpox in 1980. Like COVID-19, the smallpox virus was transmitted from “an infected person to another person via respiratory droplets following direct face-to-face contact” which typically occurred in households and hospitals.
Surveillance and containment measures were key aspects of the campaign to eradicate the deadly virus. Even after an effective vaccine was developed, the “rigorous isolation of infected persons to break the chain of transmission, and close monitoring of patient contacts” proved to be extremely effective in areas with low vaccine coverage.
What is ‘ring vaccination’?
In some cases, it is necessary to identify not just the contacts, but also anyone those contacts have interacted with, which can be a time-consuming and challenging task. If even one contact is excluded, the virus can still be transmitted, so speed and accuracy are vital.
Contact tracing can be most effective during the initial stages of an outbreak, or towards the end when cases have dropped, and it may be more practical because taking contact tracing to scale when transmission is most widespread may be challenging for some countries.
According to the WHO, tracing contacts of contacts is important because it “captures a social network of individuals and locations that may include dwellings or workplaces, where the index patient spent time while symptomatic.” For each contact this “may be composed of an average of 150 persons.”
Ring vaccination tackles an outbreak by vaccinating “a ring of people around each infected individual” to target potential hotspots at a community level. When someone tests positive, their immediate contacts can be identified and vaccinated. The ‘second ring’ of their contacts is also vaccinated to target anyone that may have been exposed to the virus.
This typically creates logistical challenges in terms of how thoroughly to implement the strategy and the high volume of surveillance and testing resources that may be required.
In the case of COVID-19, a vaccine is not currently available and given the global scale of the pandemic, it is likely that mass campaigns and targeted campaigns for particularly vulnerable groups of people will be required.
What are the challenges for contact tracers?
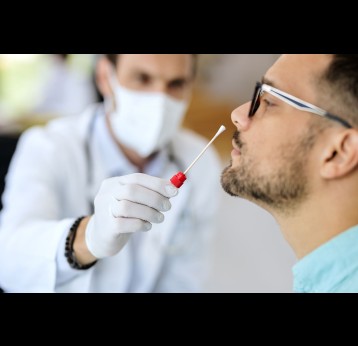
Contact tracing is a labour-intensive task that can expose frontline workers to a high risk of infection. In order to limit the transmission of a virus, contact tracers visit infected patients at their homes and complete a case-base investigation form. These forms typically include the name, age, address and occupation of the patient, as well as a list of anyone they have recently come into contact with.
Besides an increased risk of infection, contact tracers also have to contend with a fear of infection, mistrust within communities, and complex contact lists.
In some cases, as with Ebola, widespread mistrust fuelled by misinformation can make contact tracers targets within communities, and this has led to families sometimes refusing entry to their homes. “In some communities, we were targeted, because people felt that we were trying to make up a story that their relatives had Ebola. Many were in a state of denial,” says Emmanuel Lansana, one of the lead contact tracers during the Ebola outbreak in Liberia.
Read our interview with Emmanuel Lansana for his account of what it takes to be a contact tracer – and the many dangers and challenges involved.
Looking to the future
With COVID-19, contact tracing technologies like mobile phone apps are now also being trialled to help identify hotspots. This technology could help – provided privacy and security concerns are respected – to quickly notify people who may have been infected. For example, if a group of people went to a gym class and someone tested positive, all members could potentially be notified, informing them that they may be at risk, and should therefore self-isolate and get tested.
This information can then potentially be used to inform government policy as lockdown measures are gradually lifted, as it can provide important insights into whether certain types of business should remain open, or whether the data suggests they pose a greater risk of transmission.
Many of these digital tools are still being developed and deployed. Read our explainer on how the technology in our pockets can track COVID-19.