Nigeria's frontliners are learning fast to get ahead of mpox
Health workers, public agencies and community volunteers are scaling up measures to contain and cure mpox in Nigeria.
- 19 September 2024
- 8 min read
- by Afeez Bolaji
The isolation ward of the Niger Delta University Teaching Hospital (NDUTH) was unusually calm that afternoon in early September. Save for two nurses periodically shuttling up or down the corridor, the room was still.
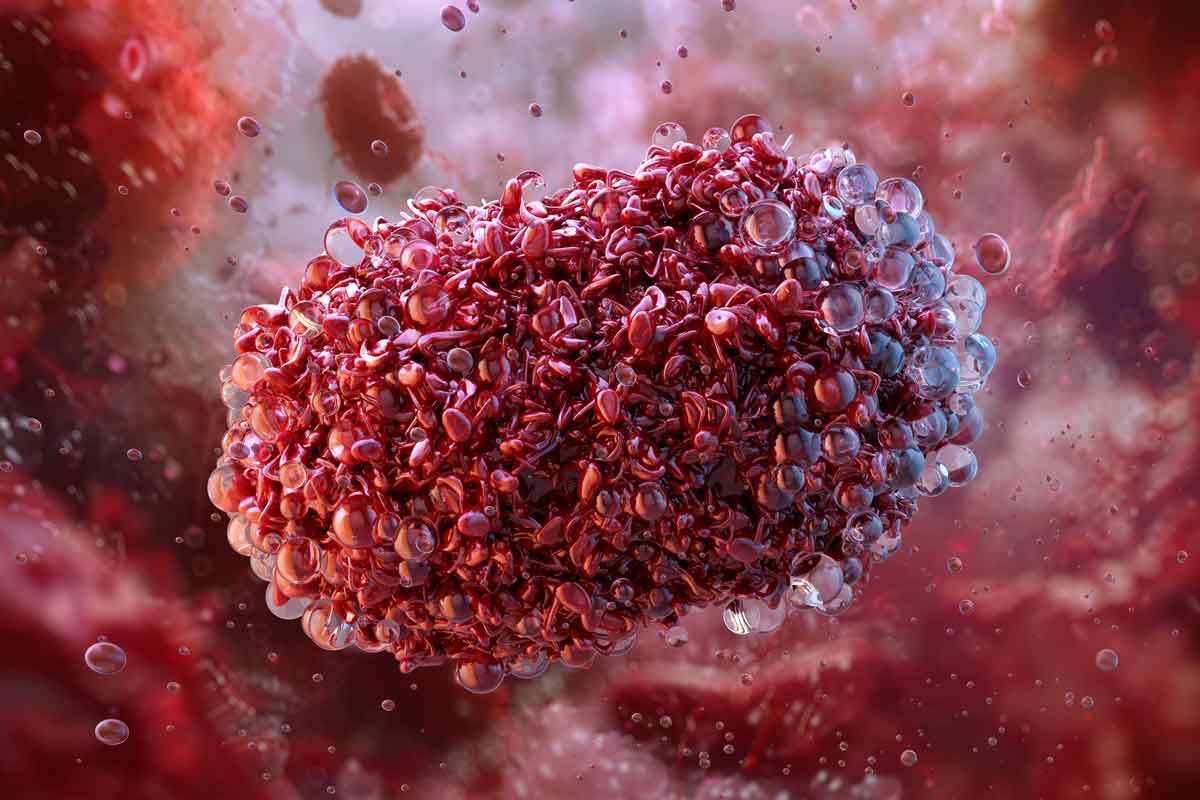
Deep inside the expansive hospital complex in southern Nigeria’s Bayelsa State, the isolation ward has recently exclusively admitted patients infected by mpox, formerly known as monkey pox – a viral disease that causes skin lesions, headaches, body pain, fever and sore throats, and which has proven deadly in at least 738 cases this year in Africa alone.
The nurses on the ward are members of a frontline team led by Professor Dimie Ogoina, NDUTH Chief Medical Director, infectious disease physician, and chair of the committee of independent experts whose recommendation underpinned the World Health Organization’s (WHO’s) declaration of mpox as an international public health emergency this past August.
Since the beginning of the year, mpox has been spreading across borders at unprecedented rates, infecting just short of 28,000 people in 15 African countries as of 16 September. Nigeria has confirmed 67 mpox cases in 23 states and the Federal Capital Territory – a total of 1,031 cases nationwide are suspected, but unconfirmed by the laboratory.
Vaccines on standby
Half a million doses of mpox vaccines have been secured for deployment in 2024, Gavi announced this week.
“We are committed to working with affected governments and our partners to turn these vaccines into vaccinations as quickly and effectively as possible,” said CEO Dr Sania Nishtar in a statement.
Over time, the Vaccine Alliance plans to build out an mpox vaccine stockpile, making doses available to ship out at shortest notice. That, however, depends on the success of Gavi’s ongoing fundraising drive for the period 2026–2030.
Six of the confirmed mpox patients were from Bayelsa, one of the states placed on high alert.
Health authorities and frontline responders, including Ogoina's team, are doubling down to curb the spread of the outbreak, which has been declared an emergency at both the continental and global levels, and to save the lives of people who have already been exposed to the virus.
Ogoina’s team successfully managed four cases between June and August. "The four patients have fully recovered, and their lesions are completely gone. We currently have a patient who is rapidly responding to treatment," Ogoina told VaccinesWork.
“2017 was a big learning experience for me. There were a lot of uncertainties about the disease, and it created anxieties. Many frontline health workers were afraid of getting infected. It took a lot of effort to convince them to participate.”
- Dimie Ogoina, physician and leading mpox expert
Learning how to heal mpox
Renowned for spotting the first confirmed mpox case after 38 years of an outbreak in Nigeria in 2017, Ogoina says lessons learned from encounters with several mpox patients in the years since have shaped how his team manages cases in the current outbreak.
"Seeing me attend to the patients inspires my junior colleagues," Ogoina says, explaining that he makes a policy of leading from the front.
"2017 was a big learning experience for me. There were a lot of uncertainties about the disease, and it created anxieties. Many frontline health workers were afraid of getting infected. It took a lot of effort to convince them to participate. We had to use incentives and boost their confidence through training and capacity building," he adds.

The patients were worried, too. One committed suicide due to fear and stigma, Ogoina recalls, and morticians were afraid to handle the corpse.
"We did emergency training for them. We also guided the family on the burial of the corpse and managed a lot of misinformation," he says.
The suicide proved to be a learning catalyst for Ogoina to better understand the psychosocial dimensions of any successful mpox response. That experience has encouraged him to devise creative ways of helping the patients cope mentally during their recovery period, which he says ranges from seven days to eight weeks, depending on the severity of the case.
"The care begins with allaying patients’ fears and making the isolation environment friendly for them. We also build their confidence by giving them examples of people who have recovered without significant scars or disfigurement.
"We manage the disease symptomatically, looking at skin eruptions, fever, sore throat, and itching and caring for them accordingly. If there is a secondary infection or complication, we treat it immediately.
"Anytime I have an mpox patient, we exchange phone numbers, and they call me if there is any issue. If there are challenges, I inform them and appeal to them to be patient. We had a patient that stayed up to two months because of skin eruptions that evolved into extensive ulcers, which required repeated care before healing.
"I also sensitise my colleagues not to stigmatise the patients knowingly or unknowingly, and I encourage them to treat [patients] with empathy. The situation became so difficult when one of our doctors got infected, but we managed it," Ogoina reveals.
Infected twice on duty
The infected medic was Dr Oru Inetsol. When he joined the team, the fear of being infected overwhelmed him, but he soon overcame it with the requisite skills and knowledge about the disease. Surprisingly, he woke up one morning with fever, body pain and weak legs. Two days later, rashes began to appear on his skin. He eventually tested positive for mpox.
"I had lesions all over my face and body, and they were itchy. I also had a sore throat. It wasn't a palatable experience. Sometimes, it was difficult to sleep at night because of the severity of the itching. My colleagues came to treat me at home. I recovered after about two weeks without any residual lesions," he told VaccinesWork.

Inetsol returned to work afterwards, exuding more confidence than before. He believed a re-infection was highly unlikely, having gained some level of immunity from the first episode. About that, he was wrong. He got infected again about three months later.
"It was abnormal to be infected twice, so I became more careful after the second infection. I'm now in the cardiology department, but whenever my service is required, I will still attend to mpox patients," he explains.
Everybody – human and animal – counts in an emergency response
To prevent the spread of zoonotic diseases like mpox, experts recommend the One Health approach that factors in mutual relationships between human health, animal health and the environment they share. The approach advocates collaboration among professionals across health disciplines and promotes community engagement.
The Nigeria Centre for Disease Control and Prevention (NCDC) is already embracing this method. In October 2023, it launched a multi-disciplinary research project on mpox case management, outbreak prevention and control. The research, expected to be concluded in 2025, focuses on clinical characteristics and the natural history of the disease, and One Health study “to increase understanding of the dynamics of infection and transmission in the Nigerian context.”
“We are studying mpox to deploy the right advocacy […] For now, we are sharing flyers on ways to prevent mpox and its symptoms. We have always been encouraging safer sexual practice.”
- Sunday Haruna, The Association of Positive Youth Living with HIV in Nigeria
At the sub-national level, some health agencies are also scaling up mpox response through community engagement. For instance, the health ministry in Akwa Ibom State – another high-alert area – works with community volunteers to report suspected cases to focal persons in health centres in their domains, says Samuel Etuk, the state’s disease surveillance and notification officer.
“The focal persons will in turn report to the local government disease surveillance and notification officers for an onwards report to the Ministry of Health,” Etuk revealed at a recent press conference in Akwa Ibom, where five mpox cases have been confirmed.
Everyone in the health sector must come together to tackle mpox under the One Health scheme, said Dr Moses Arokoyo, President of the Nigerian Veterinary Medical Association (NVMA). The association has begun grassroots campaigns using printed pictorial materials to sensitise the public to the spread and prevention of the disease, he reveals, but more needs to be done.
“The federal government must rejig the national rapid response team to ensure adequate inclusion of veterinarians for knowledge-based innovative solutions and global best practices in the spirit of One Health. The NVMA is very much ready to partner with the government in a mass vaccination campaign to safeguard our livestock. Keeping them safe ultimately means public health safety,” says Arokoyo.
The Association of Positive Youth Living with HIV in Nigeria (APYIN) has also keyed into the response after the National Agency for the Control of AIDS (NACA) disclosed recently that mpox poses higher risks to people living with HIV because of their compromised immune systems.
“We are studying mpox to deploy the right advocacy. We are working with NACA. Once we have a complete understanding of the disease, we will take up the sensitisation and engage our state coordinators. For now, we are sharing flyers on ways to prevent mpox and its symptoms. We have always been encouraging safer sexual practice," says Sunday Haruna, APYIN national coordinator.
A public health expert and consultant at the University of Port Harcourt Teaching Hospital, Professor Best Ordinioha, kicks against killing and consumption of wild animals, locally talked about as the bush meat trade
He advises that the at-risk population, including hunters, must be vaccinated as the government prepares to administer the 10,000 doses of Jynneos vaccine donated by the United States.
“There should be increased community mobilisation and health education. Case reports should be encouraged, and people need to be properly informed about the disease. Rapid diagnostic tests should also be made available so that medical lab scientists can conduct more tests," Ordinioha adds.








