HPV vaccine cuts risk of cervical cancer by two thirds in New Zealand
Ramped-up HPV vaccination and self-testing could bring the country within reach of a cervical cancer-free future.
- 26 March 2025
- 3 min read
- by Priya Joi
The first-ever study of HPV immunisation in New Zealand showed that the women who had been given the HPV vaccine were 68% less likely to develop cervical cancer than those who had not been vaccinated – and this benefit was seen equally in Māori, Pacific, Asian and New Zealand European populations.
This vaccine impact falls within the previously reported range of real-world effectiveness of the HPV vaccination, which stands at 68%–86% among girls and women aged 19 years or younger.
HPV vaccination was introduced in New Zealand in 2008, but coverage with the cancer-blocking jab is still lower than recommended. According to the World Health Organization’s global elimination strategy for cervical cancer, 90% of 15-year-old girls should be fully vaccinated with the HPV vaccine.
2021 data from New Zealand’s HPV vaccination programme shows that the coverage with the first dose is 68%, but this drops to 48% by the last dose – meaning that it stands at half of what WHO recommends.
The new data is an encouraging push for New Zealand to work towards cervical cancer elimination, say the researchers, who published their findings in the March 2025 issue of The Journal of the Royal Society of New Zealand.
Inequitable cancer screening
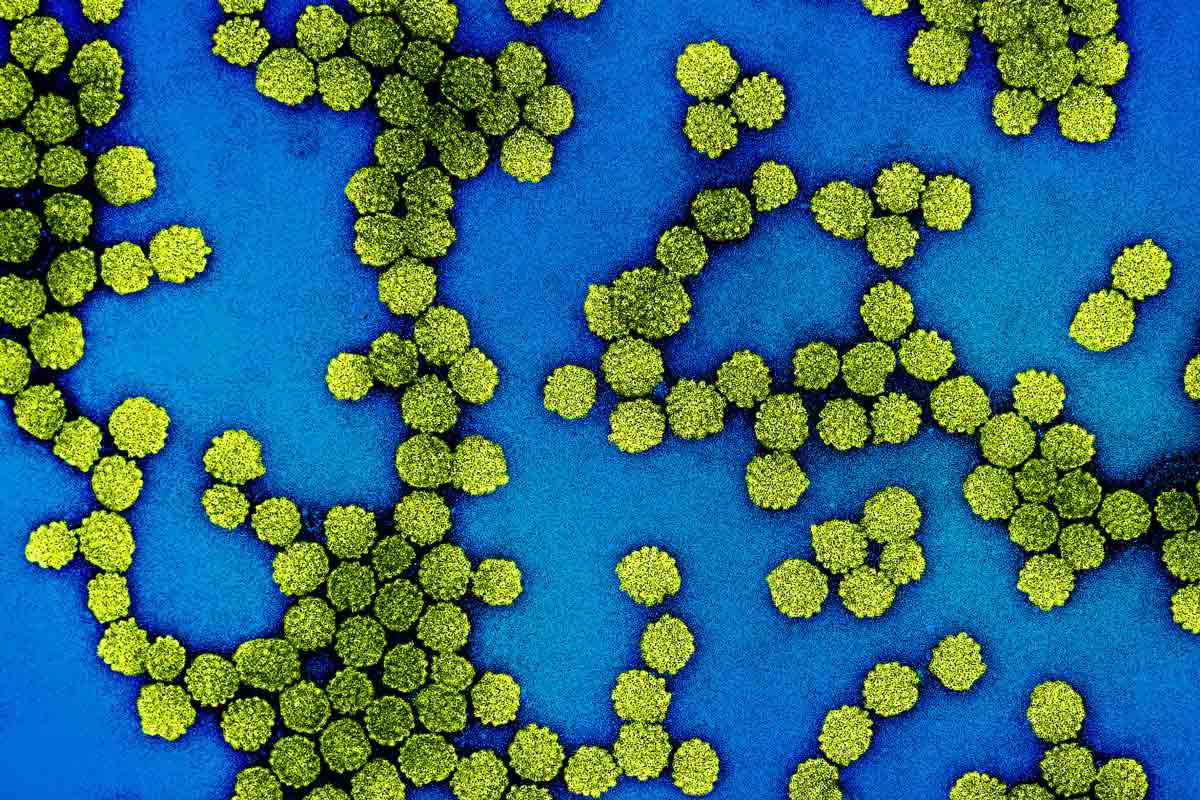
Human papillomavirus (HPV) is the cause of 95% of cervical cancers and some throat and anal cancers. Most of the women who become sick and die of cervical cancer live in low- and middle-income countries.
While New Zealand launched a national cervical screening programme in 1990, coverage has been inequitable, and as a result, cervical cancer incidence has been higher among Māori and Pacific peoples.
Per 100,000 females per year, cervical cancer distribution is uneven, with 9.1 cases in the Māori population, 8.4 in Pacific communities and 6.2 in New Zealand European people.
A 2022 study explained that for Māori women, barriers to cervical screening included lack of time or other commitments, fear of discomfort or pain, and the fact that some Māori women consider the vagina to be tapu (sacred) and, therefore, in some cases, screening caused feelings of embarrassment.
Have you read?
The revolution of self-testing
Encouragingly, self-testing for HPV is starting to make screening easier and more appealing.
When asked, 61.2% of Māori women said that they would prefer an HPV self‐test to either a clinician‐administered HPV test or conventional screening and 73.3% said they would be likely or very likely to self‐test if it were offered.
The study found that when offered it, most women found the self‐test kit easy and convenient to use and didn’t find it painful, uncomfortable or embarrassing.
In 2023, New Zealand changed its cervical screening policy to HPV testing with the option of a self-test swab. As self-testing has been rolled out relatively recently, it’s too soon to tell what its impact will be, but health experts expect that the DIY approach will make access to testing easier and more equitable, which should help drive down cervical cancer rates.
One of the authors of the current study, Prof Bev Lawton, director of the National Centre for Women’s Health Research Aoteara at Victoria University of Wellington, has long been an advocate for self-testing. “Whoever they are, Māori or non-Māori, they much prefer to take control and they don’t want to have a speculum if they don’t need to,” Lawton said.
A combination of self-testing and HPV vaccination could put New Zealand on the road to cervical cancer elimination.