Common cold could explain why some people never seem to get COVID-19
A recent cold is no substitute for a COVID-19 vaccine, but lingering immunity from one might protect a lucky few.
- 14 January 2022
- 4 min read
- by Linda Geddes

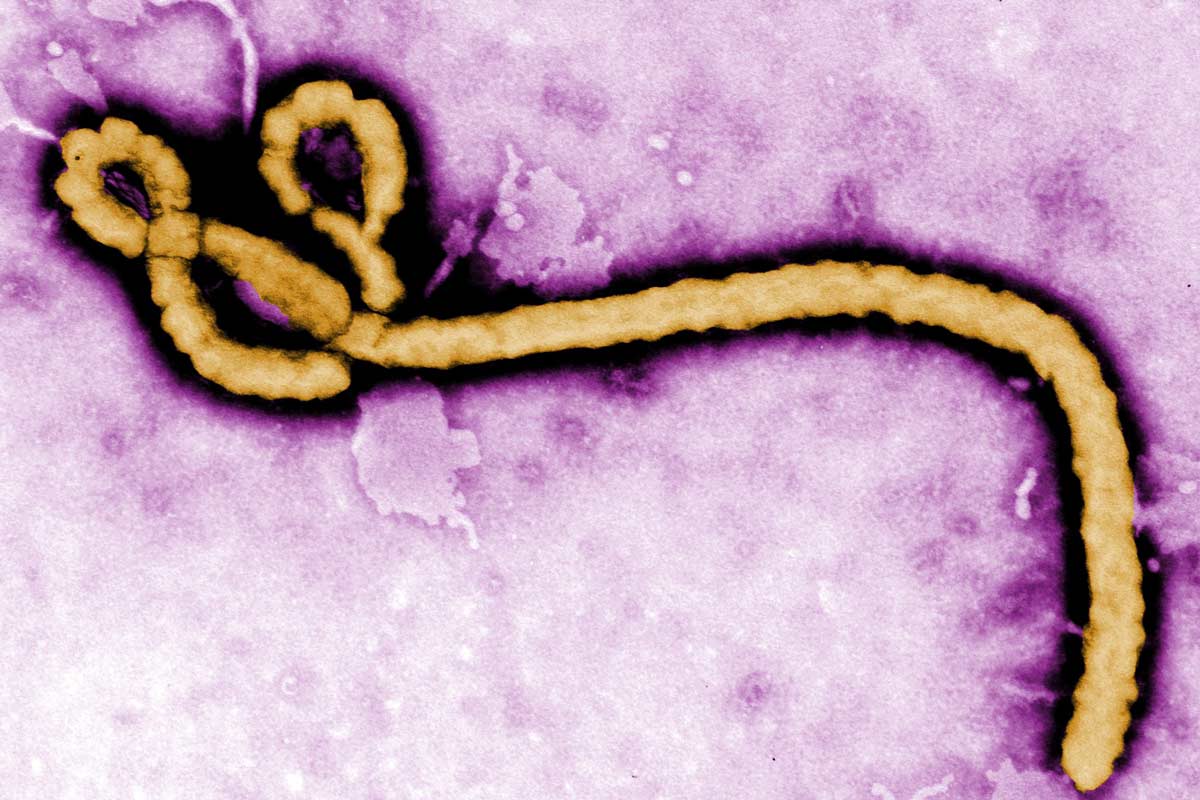
COVID-19 is caused by a family of viruses called coronaviruses – which also cause around 10-15% of common colds. New research suggests that people with higher levels of immune cells – called T cells – caused by infection with common cold coronaviruses may be less likely to become infected with SARS-CoV-2.
The research, published in Nature Communications, is one of several recent studies that are helping to unpick how our previous responses to viruses help shape our future responses to related ones.
None of this means that if you’ve recently had a common cold you are as protected against COVID-19 as if you had taken the vaccine.
T cell army
T cells form part of the immune system that kicks in several days after we first encounter a pathogen. They help our body remember the threat, meaning we respond faster the next time. Although they don’t stop viruses such as SARS-CoV-2 from infecting cells, T cells can help destroy infected cells.
T cells don’t only recognise the pathogen they’ve encountered before, but related ones as well. Throughout the COVID-19 pandemic there have been hints that exposure to other coronaviruses – including those that cause some common colds or other respiratory illnesses – might affect people’s immune responses to SARS-CoV-2. For instance, some studies have suggested that T cells from individuals who haven’t been exposed to this particular coronavirus can recognise certain parts of it.
The new study suggests that individuals harbouring such cross-protective T cells could be less at risk of testing positive for SARS-CoV-2 if someone close to them is infected with it.
Cross-protection
Starting in September 2020, Rhia Kundu at Imperial College London and colleagues recruited 52 individuals who lived with someone who had just tested positive for COVID-19, but had never knowingly had the infection themselves. They took blood samples from these people within 1-6 days of being exposed to the virus, and analysed levels of pre-existing T cells triggered by previous common cold coronavirus infections, which also recognised proteins from SARS-CoV-2.
Have you read?
Individuals with higher levels of these cross-reactive T cells were less likely to catch COVID-19 from the infected people around them, compared to those with low levels of such T cells.
Stopping infection
In similar, but separate research, Mala Maini and colleagues at University College London analysed blood samples taken from UK healthcare workers during the first half of 2020, most of whom wore protective equipment, and never tested positive for COVID-19 or antibodies to the virus.
In some of these individuals, they identified a tell-tale protein linked to COVID-19 infection, plus T cell responses to SARS-CoV-2, suggesting that a strong response by pre-existing T cells may have enabled them to stop an early COVID-19 infection before the virus could take hold, meaning they never tested positive.
Possibly, previous common cold exposure may have given these individuals a head start against COVID-19, tipping the balance in favour of their immune systems eliminating the virus before it could start to replicate, the researchers said, although there’s no conclusive proof of this yet.
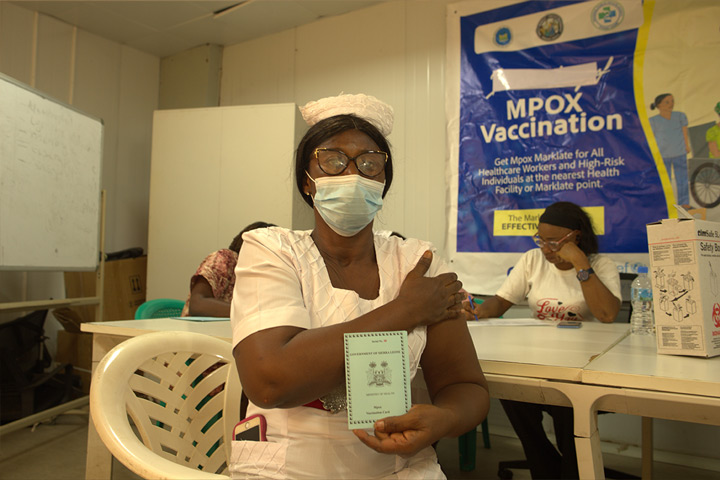
We still need vaccines
None of this means that if you’ve recently had a common cold you are as protected against COVID-19 as if you had taken the vaccine. For one thing, only a small percentage of colds are caused by coronaviruses. Second, “It seems unlikely that everyone who has died or had a more serious [COVID-19] infection, has never had a cold caused by a coronavirus,” said Dr Simon Clarke, associate professor in cellular microbiology, at the University of Reading, UK, who was not involved in the research. Neither do we know how much protection common cold coronaviruses might confer, nor for how long. The only reliable way of ensuring you’re well protected against COVID-19 is to get vaccinated against it.
Importantly though, the proteins that these cross-reactive T cells recognise tend to be hidden away inside the virus, and are much less susceptible to change than the spike protein found on its surface. A better understanding of this process could help to identify new targets for universal coronavirus vaccines – ones that not only protect against new COVID-19 variants, but future pandemic coronaviruses as well.