Preparing for the unknown: how the world can get ready for the next pandemic
South African infectious diseases expert Professor Salim Abdool Karim explains how the world can prepare for the next pandemic – even if we don’t yet know what it will be.
- 18 June 2024
- 9 min read
- by Mandy Collins
As the COVID-19 pandemic unfolded, South Africans got used to seeing the face of Professor Salim Abdool Karim on their television screens as he explained the science behind the SARS-CoV-2 virus, its various mutations, and the global response to it.
In the midst of crisis, his appearances had a calming effect. In person, too, there is something very reassuring about the public health physician, epidemiologist and virologist, who played a leading role in both the AIDS and COVID-19 pandemics at home and abroad. Talking to him feels a bit like talking to a favourite uncle. His manner is warm, and he has the rare ability to take complex scientific concepts and make them both comprehensible and unintimidating. He signs his emails simply, “Slim,” which is how he is known to friends and colleagues.
His unassuming demeanour belies the strings of accolades and qualifications to his name. He is respected internationally in his field, and in 2022, was appointed as a Special Advisor on pandemics to Dr Tedros Ghebreyesus, Director-General of the World Health Organization (WHO). His task? To be part of a team helping the global health body to prepare for the next pandemic.
“The likely scenario is that it will be a new virus and we will have no immunity to it.”
“I report directly to Dr Tedros, and I spend about 10–20% of my time – about half a day a week – supporting WHO in this area,” says Abdool Karim. “So, I spend some of that time going to WHO in Geneva, or to Berlin where the WHO Pandemic Hub is located.
“My role is purely advisory; I have no real authority,” he says with a smile. “I just have to whisper scientific advice into people’s ears. They’re perfectly entitled to take the whisperings or not.”
He’s done a lot of expert whispering in his career: at the height of the COVID-19 pandemic, his main role was to advise the South African Government, and later the Africa Centres for Disease Control and Prevention (Africa CDC) of the African Union. But he has also advised and briefed many other governments, including the US and UK.
Abdool Karim says pandemic preparedness policy in South Africa goes right back to the formation of the National Advisory Group on Immunization (NAGI) in 1993, when the African National Congress (ANC) was still a liberation movement, and had not yet taken the reins as the country’s governing party. “A joint committee comprising government officials and representatives of the ANC was set up to start preparing for a flu pandemic,” he says. He was among those appointed to serve.
“We set about devising a flu pandemic preparedness plan,” says Abdool Karim, “because the whole world was anticipating that in either 1994 or 1995, we would have a flu pandemic. Flu comes in cycles, and it was due to hit again.”
Under the leadership of Professor Barry Schoub, director of South Africa’s National Institute of Virology at the time, the committee put a structure and a set of activities in place, planned surveillance measures, and drew up plans for the acquisition of vaccines. “We also told the government that the main thing we needed was [antiviral drug] Tamiflu, because it was the key thing that would save lives of the elderly,” he recalls. “We suggested they buy it early – as there would not be stock available for South Africa when there is an actual flu pandemic – and stockpile it, which they did.” As it turned out, the anticipated flu pandemic never materialised, but for the time, he says, that was a quite a farsighted plan.
“When it came to COVID-19, the situation was very different,” he says. “Almost everybody was caught napping. We were never prepared for a respiratory virus with a reproductive rate of around three, and one for which we had zero immunity. We had no available vaccines or treatments that applied. And we should have been better prepared.”
Abdool Karim says there were several warnings that coronaviruses were creating epidemics of respiratory illness – the first SARS outbreak in China and Hong Kong around 2002, and then the Middle East Respiratory Syndrome (MERS) in 2012. “SARS was not a very infectious virus, but we knew in 2002 that coronaviruses could jump into humans via an intermediate host, and they could cause an epidemic-like situation. MERS was also a low infectivity virus, so it could be contained, but we could already see that every eight to ten years, another coronavirus would emerge.” And it did, bang on schedule.
“Add eight years to 2019, and we need to be ready for 2027, just in case,” he says. “Nobody has a crystal ball, but to say that you don’t think it’s going to happen is a bit foolhardy, because it’s already happened, so we have to work on the basis that it’s likely it will come around again.
“We could already see [in 2012] that every eight to ten years, another coronavirus would emerge … Add eight years to 2019, and we need to be ready for 2027, just in case. Nobody has a crystal ball, but to say that you don’t think it’s going to happen is a bit foolhardy, because it’s already happened, so we have to work on the basis that it’s likely it will come around again .”
“The question that we all have to ask is, will we have existing immunity? And the answer to that is, we don’t know. But the likely scenario is that it will be a new virus and we will have no immunity to it.”
A three-pronged approach
The challenge is preparing for something that is, as yet, undefined. “When you’re preparing for that kind of scenario, you have to prepare on the basis of three key elements,” says Abdool Karim. “First, you have to have surveillance in place, because the best time to prevent a pandemic is before it happens.
“Second, you need the government machinery in place with a plan – ensuring there’s a command-and-control structure, that there are finances made available, that there are teams that can make decisions, that there’s a structure for funding. And that plan should preferably be supported by legislation, as there are many legal implications of pandemic control measures. Having a well-functioning health care system is going to be critical to implement these measures in hospitals, laboratories and in the community.
“Third, you need the ability to make and access biomedical countermeasures, and there are three key ones: the first is diagnostics, the second is vaccines and the third is treatment – not just medications, but ventilators, oxygen, and so on.”
Most countries are focusing on the latter two elements, he notes, which form part of the international pandemic accord that was supposed to be wrapped up by 24 May this year, after two years of negotiations. However, serious disagreements arose around how much product pharmaceutical companies should be required to set aside for lower- and middle-income countries in need, as well as around intellectual property rights.
“Several countries have refused to allow any language in the treaty on equity relating to intellectual property,” says Abdool Karim. “They view biomedical countermeasures as a vehicle for profiteering. The African Union tabled some language that would promote equity – but this was rejected.
“The original language said that if any country developed a biomedical countermeasure, they were obligated to make 50% of it available to an international equitable distribution mechanism, like COVAX,” he says. “But some wealthy countries didn’t view that as an acceptable approach. They want to keep it all.”
Inequity in vaccine distribution was a major challenge as the world grappled with COVID-19. Initiatives like COVAX – one of three pillars of the Access to COVID-19 Tools (ACT) Accelerator – were designed to counteract it.
Have you read?
COVAX brought together governments, global health organisations, manufacturers, scientists, the private sector, civil society and philanthropy, with the aim of providing innovative and, vitally, equitable access to COVID-19 diagnostics, treatments and vaccines.
In effect, this was a kind of forerunner to the pandemic accord currently being negotiated. “I didn’t realise how some countries actually want the inequity,” says Abdool Karim .
“When countries have chosen to be amoral in protecting and fostering a ‘me first’ approach, it’s very hard to convince them otherwise. At some level I do understand that leaders want to protect their own citizens first. But there comes a point in where you have to acknowledge that viruses don’t respect national boundaries. It’s called a ‘pandemic’ for a reason.
“No country can control a fast-spreading pandemic virus in isolation while it is spreading elsewhere in the world – as we saw with Omicron. A pandemic response must be a global response, not just a country response.”
Empowering clinicians
Returning to the question of surveillance, Abdool Karim says a robust early-warning system requires empowering clinicians, who are the first line of defence. “Almost every pandemic is identified initially by an astute clinician,” he says. “If you think about it, who identified the AIDS pandemic? It was a doctor at the US CDC who saw that there were all these requests coming in from California and New York, for pentamidine to treat pneumocystis carinii pneumonia. He saw that the patients were all gay men, and that was the first identification of AIDS in the 5 June 1981 issue of the Morbidity and Mortality Weekly Report.
“If you think about COVID-19, Drs Zhang and Li from the Wuhan District Hospital were seeing undiagnosed pneumonias and realised they were dealing with an unusual infectious disease. When Dr Li became concerned that his reports were not being taken seriously by the Wuhan district authorities, he started writing messages about his undiagnosed pneumonia cases on WeChat – so much so that the police went to his house and warned him not to spread rumours about these cases of pneumonia. But he was proven to be correct.
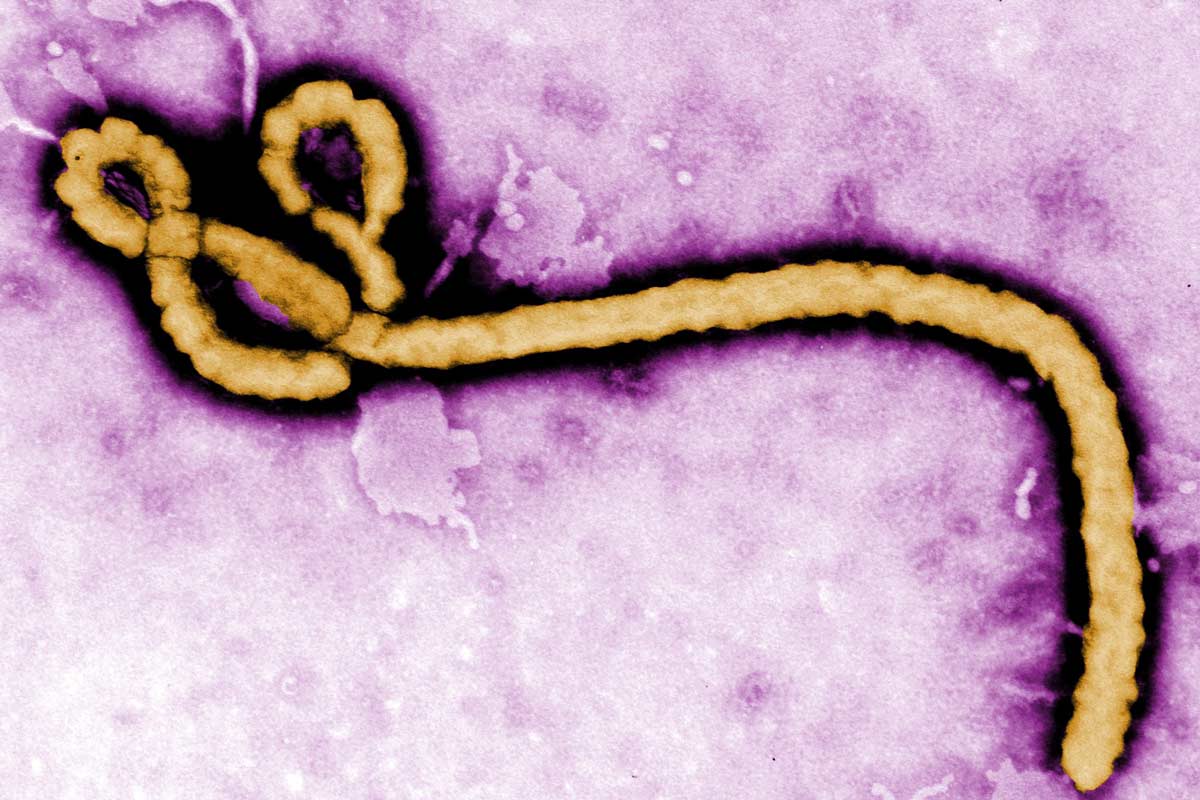
“There are many other cases of clinicians being key to early identification of epidemics and pandemics – even cases of Ebola were initially identified by clinicians in the Democratic Republic of the Congo.”
There’s a simple explanation for this, he says. When there is a new organism spreading, you don’t know what it is and don’t have a test for it, so you can’t identify it in a laboratory. You have to identify clinically that you’re dealing with something unusual, and then the labs follow later by identifying the causative agent.
“But the actual pandemic is initially picked up by clinicians. So, we need alert clinicians to pick up initial cases, and then notify the district authorities or the national infectious disease authorities as a key part of the chain for an effective early containment response.”
That’s part of what the WHO Hub for Pandemic and Epidemic Intelligence in Berlin is all about, he says. One of its programmes is working at country level with infectious disease and public health agencies, all of which have the responsibility to do surveillance, to receive notification of new illnesses, and then to act on that – to listen when doctors notice there’s a problem.
While the COVID-19 pandemic brought immense challenges, the knowledge that experts like Abdool Karim are already working behind the scenes to prepare for the next one is comforting. And hopefully, by prioritising practical preparedness measures and fostering international cooperation, we can face future outbreaks with not only resilience, but a proactive, equitable approach, safeguarding not only public health, but building a more secure future for all.