Malaria deaths spiked during the pandemic, study finds
The colossal strain put on health services by COVID-19 led to collateral damage that is still emerging today, according to a new study.
- 8 July 2025
- 4 min read
- by Priya Joi

A new analysis of 2020 and 2021 data shows that disruptions to healthcare services, resource reallocation and lockdown measures led to sharp increases in illness from malaria as well as mental health disorders.
Malaria saw a dramatic resurgence during the pandemic. In children under five there was a 14% spike in malaria deaths in 2020 and 2021. There was also a 12% rise in malaria-related disability-adjusted life years (DALYs) – a measure combining years of life lost due to premature death and years lived with disability.
The study, published in the British Medical Journal (BMJ), underscores the urgent need for resilient health systems that can sustain essential services during public health emergencies.
The rollback of progress in tackling diseases like malaria means that health emergencies need to be dealt with more effectively, according to the authors from Zhejiang University, Hangzhou, China.
This will mean ensuring the continuity and accessibility of essential services during health emergencies, for example through decentralisation or mobile outreach.
Calculating the difference
The authors analysed data from 2020 and 2021 from the Global Burden of Disease Study, which assessesmortality and disability across different populations and over time, providing valuable insights for health policy and resource allocation.
In this study, the researchers analysed 174 causes of disease burden for which data was available from 1990–2021, excluding COVID-19 disease, to assess the collateral damage from the pandemic.
Then they calculated differences between observed and expected rates of disease and deaths for 2020–2021 to quantify the specific impact of the pandemic.
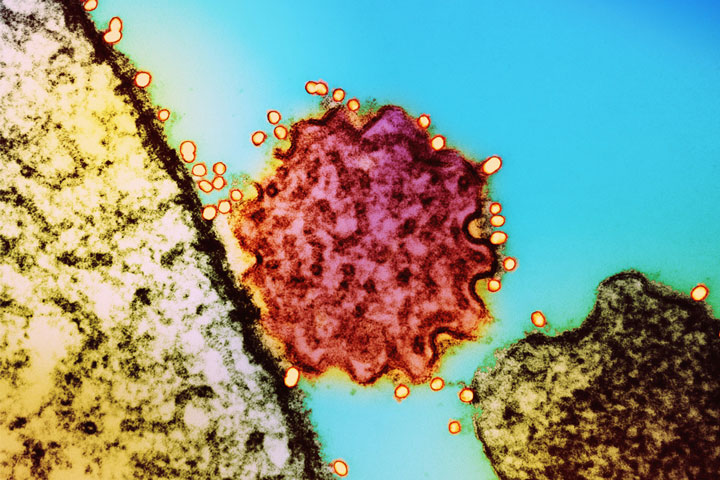
Malaria surge
Malaria saw a dramatic resurgence during the pandemic. In children under five there was a 14% spike in malaria deaths in 2020 and 2021. There was also a 12% rise in malaria-related disability-adjusted life years (DALYs) – a measure combining years of life lost due to premature death and years lived with disability.
Disruptions to prevention, diagnosis and treatment services were the primary drivers of this increase. Routine distribution of bed-nets, access to antimalarial drugs and community outreach programmes were all severely affected as health systems diverted resources to fight COVID-19.
Have you read?
According to the analysis, there were an estimated 14 million more malaria cases and 69,000 additional deaths in 2020 compared to 2019, with about two-thirds of these deaths directly attributable to COVID-19-related disruptions in malaria services.
The increase in malaria-related DALYs was particularly pronounced in young children, highlighting the vulnerability of this age group when routine health services are interrupted.
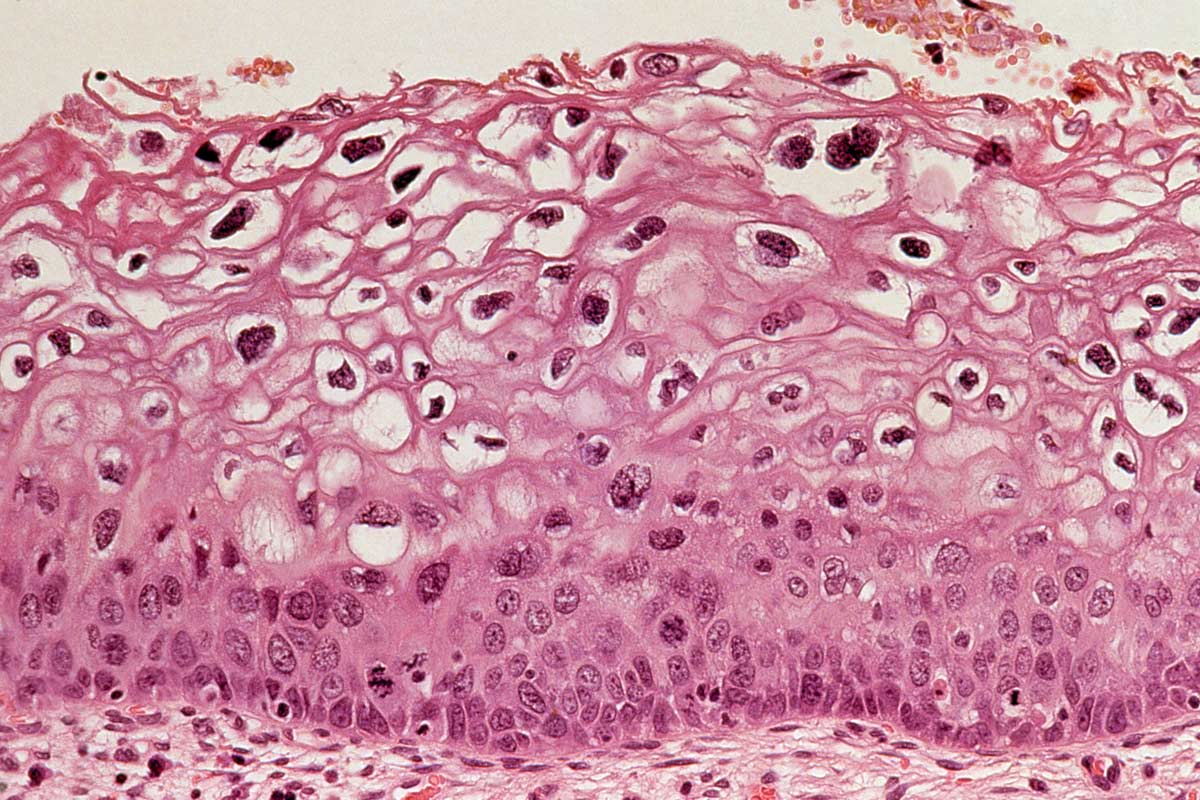
Rise in depression and anxiety
Mental health disorders also saw a significant surge during the pandemic. The prevalence of depressive and anxiety disorders rose by 12% and 14%, respectively, with the greatest increases observed among women and individuals aged 15 to 49. New cases of depressive disorders in children aged 5 to 14 rose by 23%. The rise in the burden of depressive and anxiety disorders was more pronounced in women.
This finding fits with previous data from a Lancet study showing that, in 2020, the global prevalence of anxiety and depression increased by more than 25%, with women being nearly twice as likely to be affected as men.
The fear of infection, loss of loved ones and the unpredictability of the pandemic created unprecedented levels of stress and anxiety worldwide.
Mental health disorders also saw a significant surge during the pandemic. The prevalence of depressive and anxiety disorders rose by 12% and 14%
But the BMJ authors also say that SARS-CoV-2 infection can trigger an abnormal response of the immune system, leading to chronic low-level inflammation, which could have affected the balance of neurotransmitters such as dopamine, imbalances of which can trigger a risk of depressive and anxiety disorders.
Preparing for the future
This data builds on a growing body of evidence that has exposed critical gaps in global health preparedness.
Addressing these indirect impacts by reinforcing primary care, expanding surveillance and prioritising universal health coverage will be essential to mitigate the long-term consequences of COVID-19 and other health emergencies, and to build stronger, fairer health systems for the future, the authors say.
They recommend integrating disease surveillance so that both infectious and non-communicable diseases are monitored in real time. Essential services should remain operational to ensure that routine care for malaria, mental health and other conditions continues, even during an unprecedented crisis.