A brief review of vaccinology
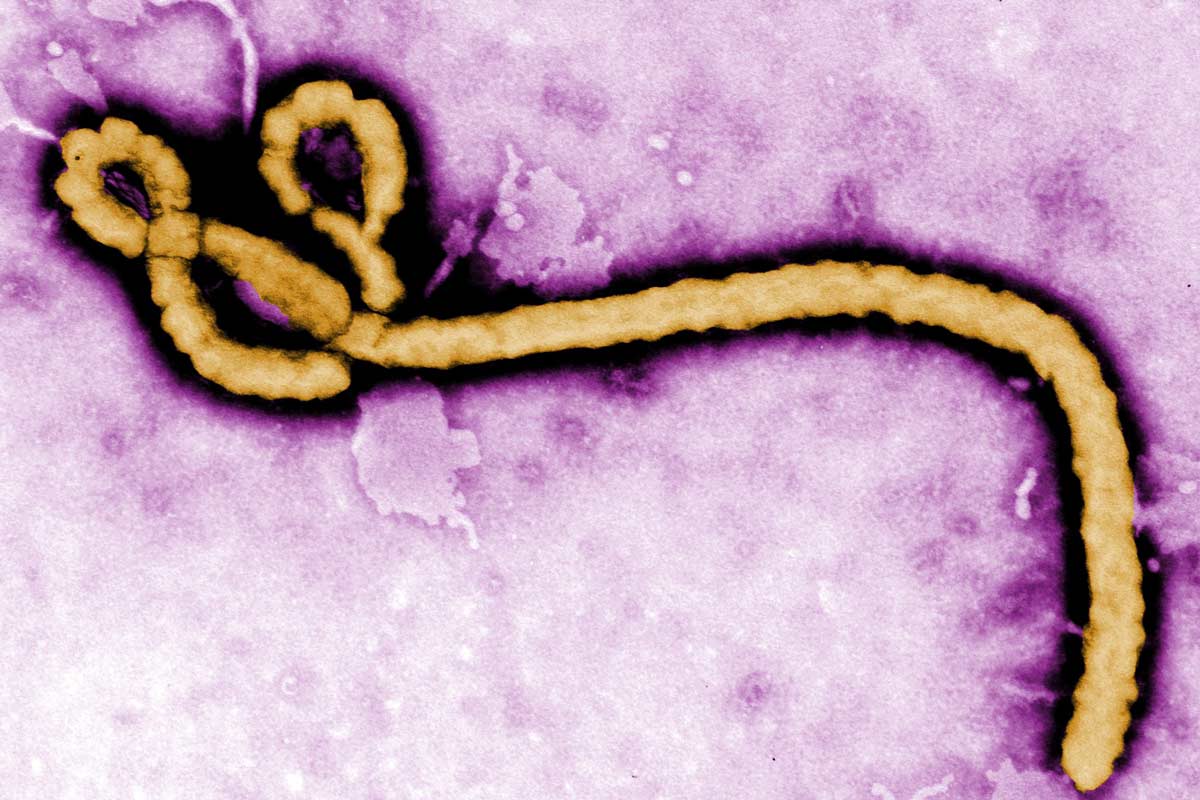
Vaccines are weakened or killed pathogens (virus, bacteria, or parasite that causes human disease) or a modified part of a pathogen. Although the vaccine does not cause disease, it helps your immune system recognize the pathogen and develop a defense—immunity—against it. This immunity can last a long time and should protect you against infection or illness in the future.
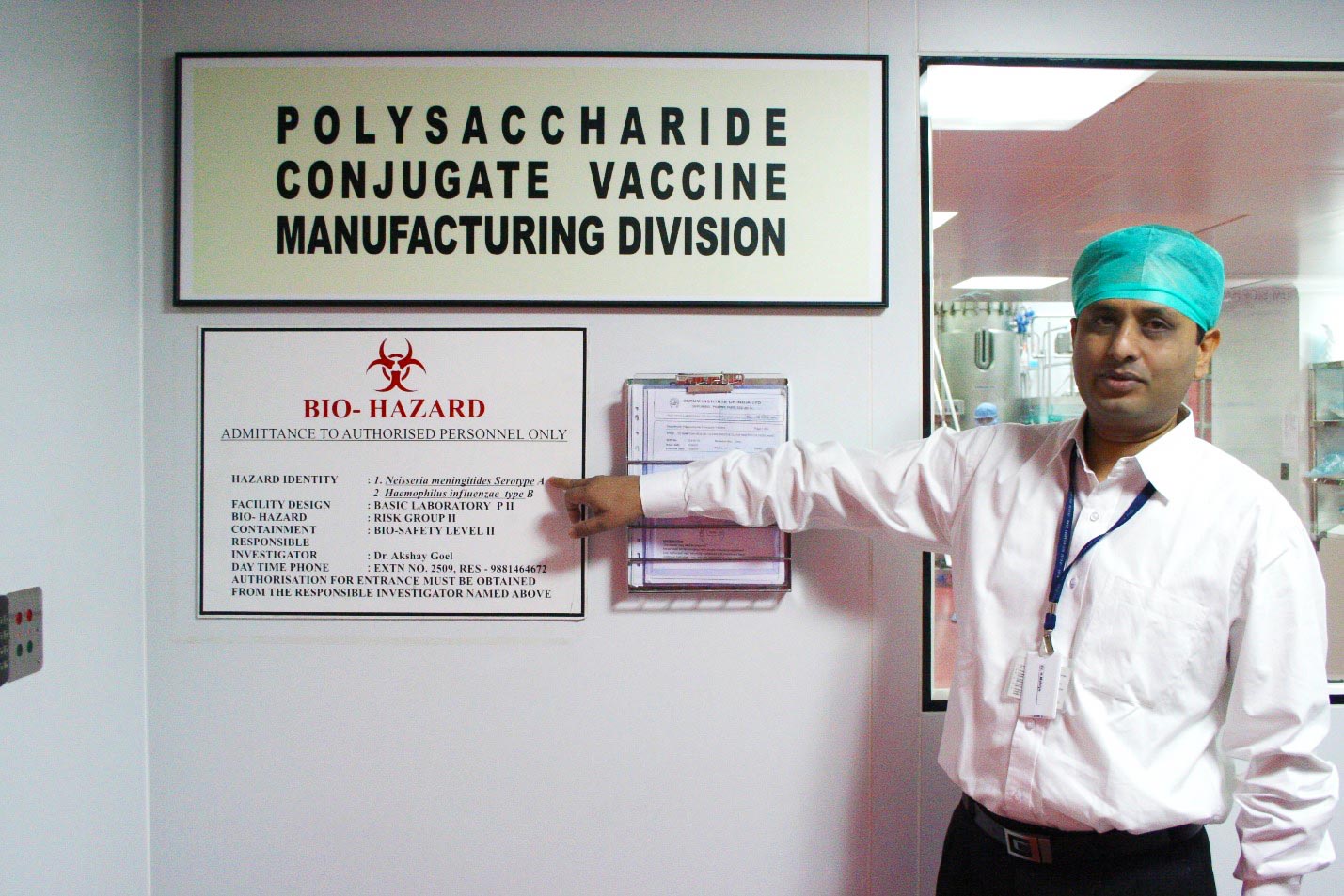
There are many ways to make pathogens into vaccines. Take, for example, typhoid, which is caused by a bacteria called Salmonella enterica serovar Typhi. One type of typhoid vaccine, called a Vi capsular polysaccharide vaccine, contains chains of identical sugar molecules (polysaccharides) from the surface of the Salmonella bacteria. This is a “subunit” vaccine because it does not contain the whole pathogen; just a part that is large enough to be recognized by your immune system.
These vaccines work well against a lot of different types of infections, but every pathogen is unique and the same modification process may not work for all pathogens. Additionally, our immune systems change as we grow. This means a polysaccharide vaccine like the current Vi capsular polysaccharide typhoid vaccines works in older children and adults, but does not work as well in infants. This leaves a large gap in protection, especially for infections that commonly occur in infancy.
A creative solution
To address this gap in protection for infants, scientists in the 1980s got creative. A polysaccharide vaccine against Haemophilus influenzae type B (Hib), which can cause meningitis and pneumonia, did not work well in infants, the most vulnerable population to Hib infection. This highlighted the need for a new vaccine that could protect infants. In response, scientists created the Hib conjugate vaccine—the first of its kind.
So, how do conjugate vaccines work? First, the polysaccharide is attached (or “conjugated”) to a more complex protein. The protein carries the polysaccharide to certain cells in the immune system to which the polysaccharide would not have access on its own. In infants, these cells are better able to develop immune protection against pathogens. Polysaccharides alone are generally too weak, too monotonous, or too small to be detected by these cells. But, by piggybacking on a protein carrier, polysaccharides gain access to important parts of the immune system and can get more easily noticed.
A vital application
Many conjugate vaccines were developed because of the need to protect infants and young children with immature immune systems. Hib conjugate vaccines were the first successful application of this technology. After the Hib vaccines proved safe and effective in protecting the youngest children, scientists applied the same design to create other lifesaving conjugate vaccines like PCVs, MenAfriVac®, and now a new type called a typhoid conjugate vaccine (TCV).
Typhoid still has a substantial and underestimated public health burden in low-income countries, causing more than 12 million cases and nearly 150,000 deaths each year. Unlike the currently available vaccines, TCVs have the potential to protect children younger than two years old from typhoid before they are exposed, have longer-lasting protection than current typhoid vaccines, and could be included in routine childhood immunization programs. That’s why my team at PATH is part of the Typhoid Vaccine Acceleration Consortium (TyVAC), a recently launched partnership to accelerate the introduction and access to TCVs.
These vaccines have already proven the power of innovation and creativity to save lives. Conjugate vaccines can now help us make strides against other childhood diseases like typhoid, and help kids around the world live up to their full potential.