6 things to know about the 100-day cough
Whooping cough or pertussis – also called the 100-day cough – is on the rise in the UK and US. Here’s what you need to know.
- 26 June 2024
- 5 min read
- by Priya Joi

Whooping cough or pertussis is an extremely contagious and serious infection that causes coughing fits so severe that it can be hard to breathe, eat or sleep. Before vaccines were developed, the disease (caused by the bacteria Bordetella pertussis) was so deadly it killed one in ten children affected – causing twice the number of childhood deaths as from measles and polio combined.
Now, falling vaccination rates in some middle- and high-income countries are seeing the disease making a worrying comeback. Here are six key facts about the disease, why it is spreading, and how it can be stopped:
1. The name comes from the distinctive whooping sound at the end of a coughing fit
The early symptoms of pertussis resemble that of a common cold, but progress to violent coughing fits that can last several minutes, punctuated with a loud, high-pitched 'whoop' as people try to draw breath. (Click here to listen to what it sounds like). These fits of coughing can go on for three months, hence the name 'the 100-day cough'.
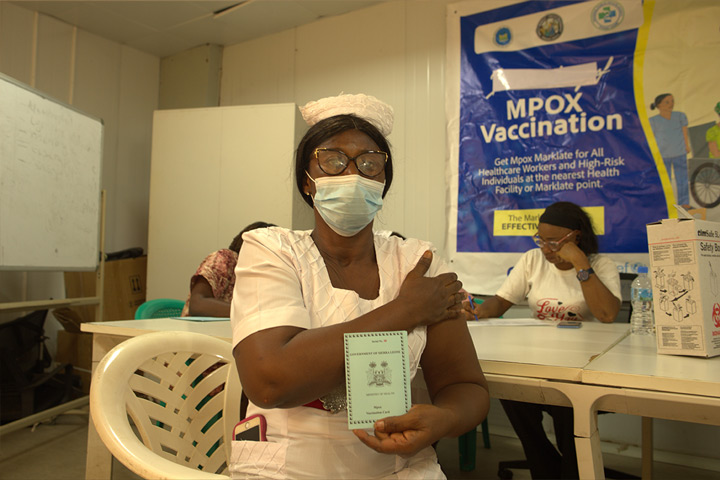
2. Vaccines are highly effective at preventing infection
The diphtheria, tetanus and acellular pertussis (DTaP) vaccine protects 98% of children from infection for the first year following the last dose, falling to 71% of children by five years after the last dose. There are other formulations of the vaccine such as the pentavalent vaccine, which also protects against hepatitis B and Haemophilus influenzae type B (Hib) disease. With Gavi’s support, this vaccine is currently available in the world’s 73 lowest-income countries.
The World Health Organization (WHO) recommends all infants have three doses of pertussis vaccine in infancy, with one booster dose in children one to six years of age. Because immunity can wane through adolescence and adulthood, some countries also offer booster doses to adolescents and adults, as well as to pregnant women to protect their newborn infants before they’ve had their vaccinations.
3. Infections are rising in countries where it had been under control
Cases of whooping cough have been on the rise in England, and this year, for example, cases in January were 556, rising to 918 in February, 1,319 in March and 1,888 cases in April. Now, monthly infections alone are higher than all of the 858 cases across the whole of 2023.
Data from the UK Health Security Agency (UKHSA) shows that the UK falls below the WHO target for 95% of under-fives to be vaccinated. While uptake of the six-in-one jab – against diphtheria, tetanus, pertussis, Hib, hepatitis B and polio – and measles, mumps and rubella (MMR) vaccine exceeded WHO targets in Scotland and Wales, for the UK as a whole, only 84.5% of under-fives had been given the jab.
In the US, meanwhile, reported cases of pertussis have increased across the country: by mid-June 2024, there were 6,275 reported cases – three times higher than against the same period in 2023 (2,113 reported cases).
4. Falling vaccination rates are sometimes more about access than hesitancy
While lower vaccine uptake is a cause for concern, some experts argue that it is not accurate to attribute this solely to parents being reluctant to vaccinate their children. While this might be the case in a small minority of parents, the overwhelming majority of parents still believe in vaccination, says US paediatrician David M. Higgins. Recent data shows that 93% of parents of kindergarten students opted to vaccinate their children with all of the state-required vaccines.
The issue, Higgins says, may be that access to vaccines has become difficult for many underprivileged families, especially in the US, where many families who were relying on Medicaid for last year lost access as the US government changed policy and shut down access for many low-income families . This means that for many families on extremely low incomes, childhood vaccines are no longer free of charge.
In the UK too, a 2019 Public Health England survey reported that 95% of parents said they had confidence in vaccinations and only 3% had refused one or more vaccines. However, according to the British Medical Journal, increasing fragmentation of childhood primary health care pathways since health system reforms in 2012 have increased the barriers that parents and carers face when trying to access immunisation for children, with a 2019 report by the UK National Audit Office noting “inconsistency in the way parents were invited and reminded to vaccinate their children”.
5. It mostly affects children and babies, but can affect people at any age
Babies and young children are most at risk – with babies particularly vulnerable in the period before they are vaccinated. This is why experts are urging pregnant women to get the vaccine, as this can protect their babies before they are old enough to receive the vaccine themselves. Although antibiotics are effective against the infection, because the early symptoms look like a common cold it can be hard for doctors to diagnose the disease early enough – in the UK, eight children have died of the disease so far in 2024.
6. Whooping cough can be confused with other viral infections that also cause violent coughing
The rise of whooping cough in the UK coincided with a particularly cold and wet start to the year, during which a range of respiratory viruses have also been doing the rounds. For instance, parainfluenza viruses can cause a persistent cough with mucus, or a barky, seal-like cough and high-pitched wheezing (croup). Adenoviruses can also cause croup. Respiratory syncytial virus (RSV), another common cause of childhood illness, causes a wet-sounding, forceful cough.
More from Priya Joi
Recommended for you