Now is the Time to Pave the Way for Equitable Vaccine Distribution
When COVID-19 vaccines become available, one of the biggest challenges the global community will face is equitable distribution. This will be the single largest vaccine deployment in history.
- 28 July 2020
- 5 min read

When COVID-19 vaccines become available, one of the biggest challenges the global community will face is equitable distribution. This will be the single largest vaccine deployment in history. Our response to the ongoing coronavirus pandemic should ensure that every person–regardless of where they live–receives a potent vaccine for COVID-19, as well as for every other vaccine-preventable disease. That response begins with a realistic look at the current vaccine cold chain infrastructure.
Delivering vaccines to communities relies on the cold chain: a complex network meant to transport vaccine vials safely from national warehouses to every health facility in a country. Navigating the journey involves transport vehicles (from bicycles to drones), specialised cooling equipment for storage, and trained personnel. Any break in the chain could cause temperature excursions that spoil vaccines. So if we want to end the pandemic swiftly, we must act now to make sure that every country, particularly the ones with the weakest health systems, has the infrastructure in place to make this possible.
COVID-19 disrupts how vaccine supply chains work, and, as a result, what is required of the global distribution system. We must tap into the data sets we already have to guide the actions we take in the coming months to get the cold chain ready. An effective plan begins with identifying the strongest and most strategically important links in the current cold chain.
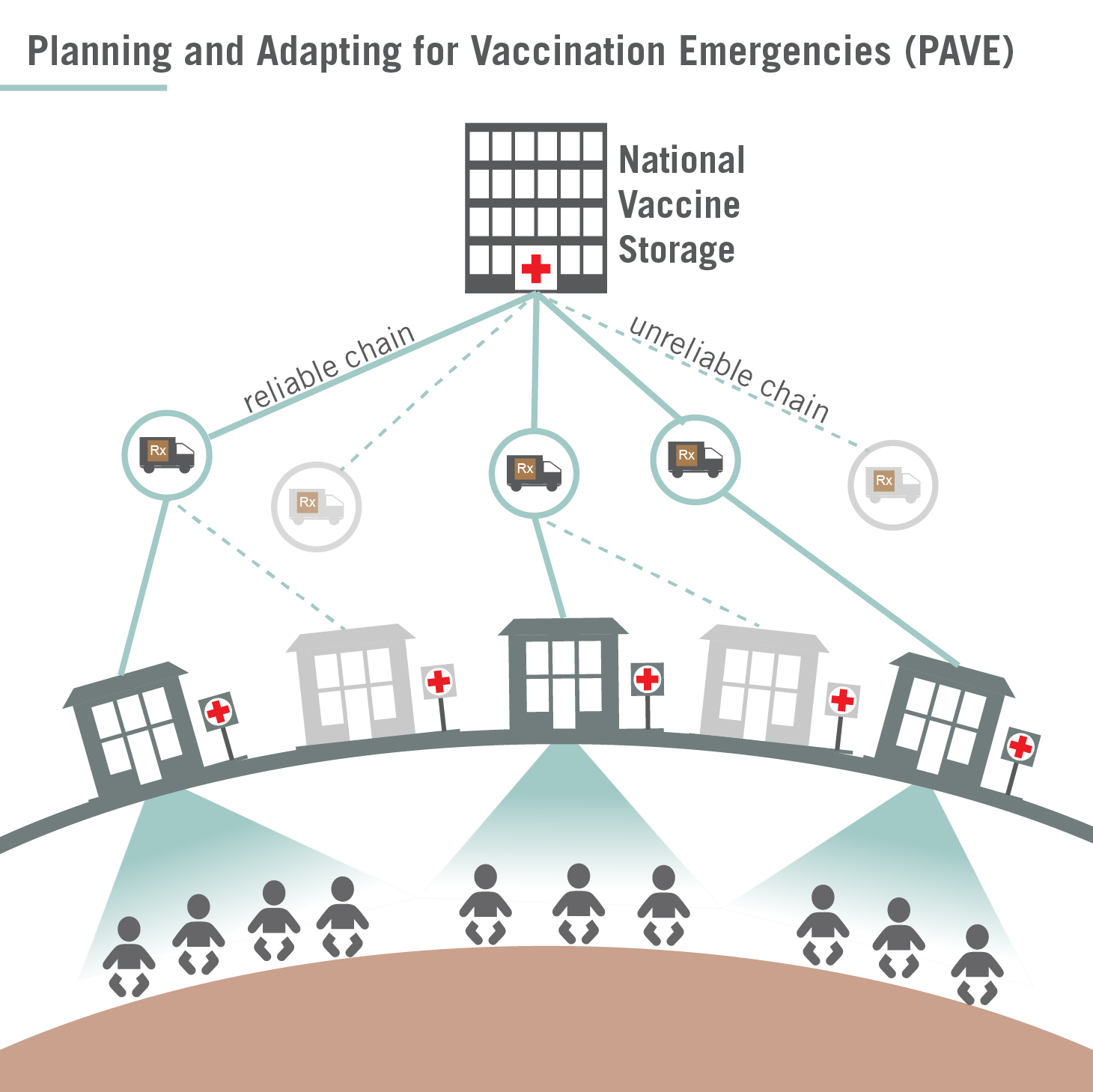
In response to COVID-19, Nexleaf Analytics, a non-profit organisation focused on data for social impact, has developed a process called Planning and Adapting for Vaccination Emergencies (PAVE). The PAVE process puts data at the center of emergency immunisation distribution planning, enabling Ministries of Health to begin with what they already know.
Applying PAVE to your cold chain planning means bringing together available data from EVM assessments, data loggers, remote temperature monitoring systems, inventories, electrification assessments and more. This way, you can identify a strategic subset of the existing vaccine cold chain to serve as the “backbone” of the country’s cold chain. Similar to an emergency exit route that designates an unobstructed pathway to exit a building, this “backbone” will become the pathway for emergency vaccine storage and distribution. Once the equipment is identified, countries can then determine and direct the resources necessary to make that pathway as strong as possible, as soon as possible.
What can decision-makers do with existing data on the current infrastructure? They can identify the weakest–and strongest–links in the cold chain. They can assess power availability and other requirements for storing more vaccines near population centres. Data-informed planning can remove unnecessary guesswork when determining each country’s unique immunisation cold chain needs.
Existing Cold Chain Infrastructure is Key to Vaccine Delivery at Unprecedented Scale
Most vaccine distribution campaigns only need to reach children as part of routine immunisation. It has taken decades to develop the necessary infrastructure for routine paediatric immunisation, and still 1 in 5 children lacks access to routine vaccines. Delivering a vaccine to every person on Earth is a hurdle we have not encountered before, and cold chain challenges will only be exacerbated by two major burdens on the horizon.
First, vaccine-preventable diseases are feared to be on the rise as a result of the COVID-19 pandemic, with the Measles & Rubella Initiative estimating that 178 million people are at risk of missing measles shots in 2020.
Second, additional demands will be placed on existing cold chains based on storage and handling requirements for the eventual COVID-19 vaccine. Several of the leading COVID-19 vaccine candidates require a second immunisation for individuals to have a robust immune response, meaning double the number of vaccines that need to be shipped, stored, transported, and administered. A few potential vaccines require an ultra cold chain, capable of maintaining temperatures of -60 °C or colder, similar to the vaccines developed in response to the 2014 Ebola outbreak in West Africa, which recently helped prevent Ebola outbreaks in the Democratic Republic of the Congo escalate and spread to other countries. It’s important not to underestimate the role of electrification in equitable vaccine distribution. Only 28% of healthcare facilities in sub-Saharan Africa have reliable electricity supply. However, there will be a tremendous increase in energy demand from additional cooling units for stationary refrigeration in national and regional distribution hubs and health facilities.
Rolling out new resources without an informed needs assessment can risk overburdening immunisation programmes. Fortunately, cold chain data has been proliferating in the healthcare system over the past decade. Now is the time to capitalise on that data. Nexleaf Analytics, an INFUSE Pacesetter, is one of the many organisations that have demonstrated how Ministries of Health can make a positive impact on their systems when they lead with data. The value of the PAVE process is that it uses existing resources and capacity, making it adaptable to vaccination efforts in response to outbreaks of known diseases and emerging diseases alike.
A Plan for the Near Future
While COVID-19 is the first global pandemic in recent history, it’s not the first viral outbreak low-income countries have encountered, and it won’t be the last. This pandemic has challenged all of us in the global health sector to tap into creativity, innovation and data to plan for the unknown. Donors, multilaterals and stakeholders alike need to follow the lead of countries when it comes to cold chain planning.
In order to protect everyone, we need more initiatives and partnerships that focus on data to embrace and work with the realities on the ground. For instance, countries can run simulation models to explore different ways to conduct mass-vaccination campaigns. Those scenarios should take into consideration what it would look like to manage the people, processes and supplies required to store and transport COVID-19 vaccines from the national level all the way to the last mile. To reach every single person, we need that comprehensive picture of cold chain logistical challenges. There is a long road to an equitable COVID-19 vaccine distribution. We must pave the way for an effective and reliable cold chain now if we want everyone protected.





