Five things we know about the Delta variant (and two things we don't)
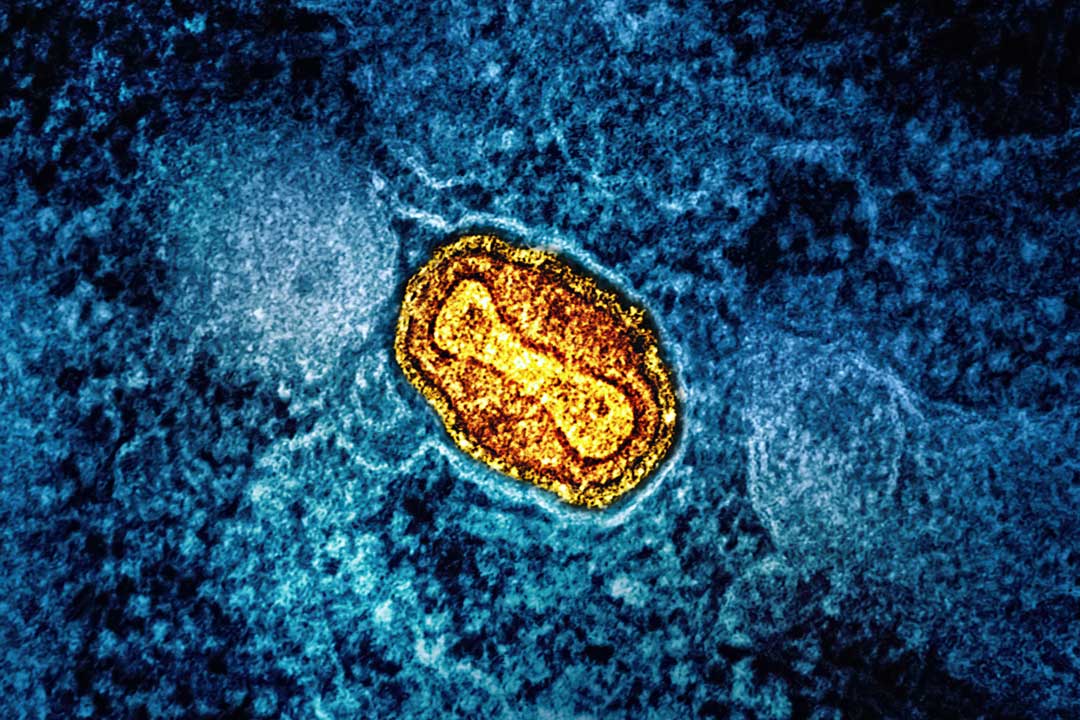
The Delta (B.1.617.2) variant of SARS CoV-2 was first detected in India and is rapidly spreading around the world. Here’s what we know about it so far.
- 15 June 2021
- 6 min read
- by Linda Geddes

1. It is rapidly spreading around the world
The Delta variant was first detected in India in late 2020, where it is thought to have contributed to the extremely high number of cases during the country’s second wave of COVID-19. As of 14 June it had spread to 74 countries worldwide, according to the World Health Organization (WHO).
The WHO’s Director for Europe has warned that Delta is “poised to take hold in the region,” as many countries prepare to ease restrictions and allow more social gatherings and travel across borders. As of 14 June, the Delta variant accounted for 10% of cases in the USA.
Two weeks after receiving a second dose, the Pfizer-BioNTech vaccine appeared to provide 79% protection against infection with the Delta variant, compared with 92% protection against the Alpha variant, the study found.
2. It appears to be more transmissible.
One country where the Delta variant has taken hold is the UK. Since the first cases were detected in February, it has rapidly overtaken the so-called Alpha (B.1.1.7) variant that was first detected in Kent, England, and which was itself 43 to 90% more transmissible than pre-existing variants of SARS-CoV-2. Delta currently accounts for more than 91% of UK COVID-19 cases, and is around 40% more transmissible than the Alpha variant, according to UK government estimates. However, other scientists have calculated it may be 30-100% more transmissible than Alpha.
Scientists are currently investigating the reasons for this apparent enhanced transmissibility. There are already some signs that small changes in the variants’ spike protein may enhance its ability to bind to the ACE2 receptor that it uses to gain entry to human cells. Another study, which has not yet been peer reviewed, has suggested that a separate mutation in the Delta variant may enhance its ability to fuse with human cells once it latches on. If the virus can latch on and fuse more easily, it may be able to infect more of our cells, which may make it easier to overwhelm our immune defences.
3. It may be associated with different symptoms
Delta is also rapidly spreading in Southeast China. Here, doctors are reporting that patients are becoming sicker and their conditions deteriorating more quickly than the patients they treated at the start of the pandemic.
Have you read?
In the UK, data from the Zoe Covid Symptom Study, where participants track their daily symptoms via a smartphone app, has also suggested that the symptoms associated with COVID-19 may be changing due to the rise of the new variant. Since the start of May, the number one symptom reported by app users with a confirmed infection has been headache, followed by sore throat, a runny nose, and fever. “Cough is rarer and we don’t even see loss of smell coming up in the top ten anymore,” said Prof Tim Spector, who is leading the study. The risk is that younger people – who are already less likely to develop severe illness - may be more likely to mistake such symptoms for a bad cold, and not self-isolate, further enhancing Delta’s spread, Spector said.
4. People may be more likely to be hospitalised with the Delta variant
Most of the scientific data that has been published about the Delta variant so far, has come from the UK, where researchers are using a rapid method called “genotype assay testing” to work out whether a positive COVID-19 sample contains a variant of concern, such as Delta, or not.
According to a Scottish study published in The Lancet on 14 June, the Delta variant is associated with approximately double the risk of hospitalisation compared with the Alpha variant. The study looked at data from 19,543 community cases of COVID-19 and 377 hospitalisations reported in Scotland between 1 April and 6 June 2021. People with underlying conditions were at greater risk of being hospitalised, it found.
5. One vaccine dose is less effective, but two doses are still strongly protective
The same study suggested that people who had received a COVID-19 vaccine were less likely to be admitted to hospital with the Delta variant compared to unvaccinated individuals - but strong protective effects were not seen until at least 28 days after the first vaccine dose.
Two weeks after receiving a second dose, the Pfizer-BioNTech vaccine appeared to provide 79% protection against infection with the Delta variant, compared with 92% protection against the Alpha variant, the study found.
Just today new data published as a pre-print by Public Health England (PHE) demonstrated two doses of the Oxford-AstraZeneca vaccine are 92% effective against hospitalisation due to the Delta variant and showed no deaths among those vaccinated. The vaccine also showed a high level of effectiveness against the Alpha variant with an 86% reduction of hospitalisations and no deaths reported. The data also suggests that vaccine effectiveness against symptomatic disease was 74% against the Alpha variant and 64% against the Delta variant.
Separate data published by Public Health England suggested that the Pfizer-BioNTech vaccine was 88% effective against symptomatic disease from the Delta variant two weeks after the second dose, compared to 93% effectiveness against the Alpha variant.
Similar to the Scottish data, PHE found that a single dose of either vaccine was less effective against the Delta variant, compared to the Alpha variant: three weeks after a first dose, the vaccines provided 33% protection against symptomatic disease caused by the Delta variant, compared to around 50% protection for the Alpha variant.
...And two things we still need answers to:
1. Is the Delta variant associated with more deaths?
There have not yet been enough deaths to systematically compare those associated with Delta and other variants, after ruling out other potential causes. As of 14 June, the UK had reported 42 deaths among people infected with the Delta variant. Of these, 23 were in unvaccinated individuals, seven were in people who had received a first vaccine dose, and twelve occurred in fully-vaccinated individuals. However, those who have received two vaccine doses in the UK tend to be older and more clinically vulnerable, making it difficult to examine the impact of the Delta variant on death rates at this stage.
2. Will we need booster doses against it?
This is also currently unknown, but it should become clearer as Delta continues to spread and more people receive additional doses of COVID-19 vaccines. Laboratory studies on the ability of vaccine-induced antibodies to neutralise the virus, post-booster dose, should also help to answer this important question.