Five charts on 15 years of the HPV vaccine
More than 15 years have passed since the first HPV vaccine introduction, and real-world evidence for its effectiveness is now well established. However the global burden of HPV-related cervical cancer has shifted to lower-income countries, where access to prevention, including vaccination, remains limited.
- 11 October 2022
- 3 min read
- by Jessica Gergen

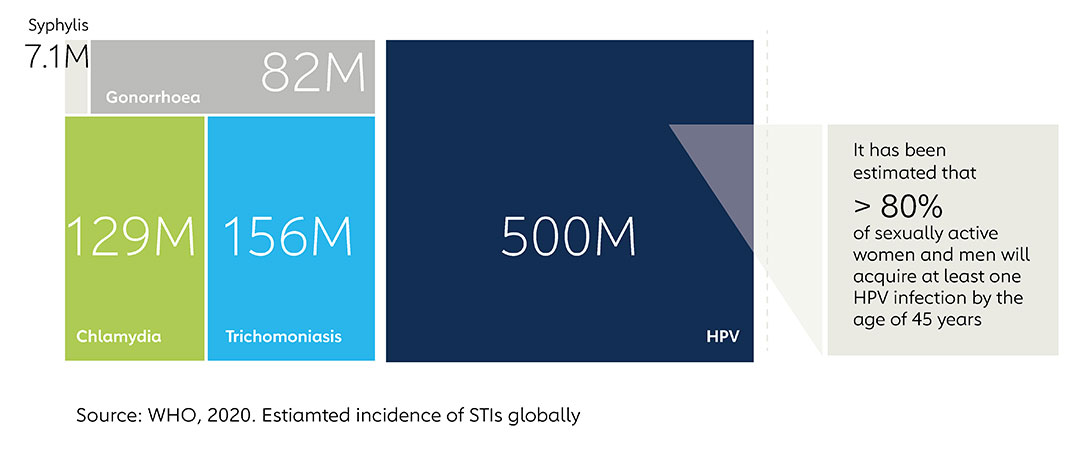
The scale of the problem
Human papillomavirus (HPV) remains one of the most common STIs globally, with an estimated 80% of men and women having acquired at least one HPV infection by age 45. While global awareness of HPV as the leading cause of cervical cancer has increased, access to preventive measures has lagged and stigma remains high.
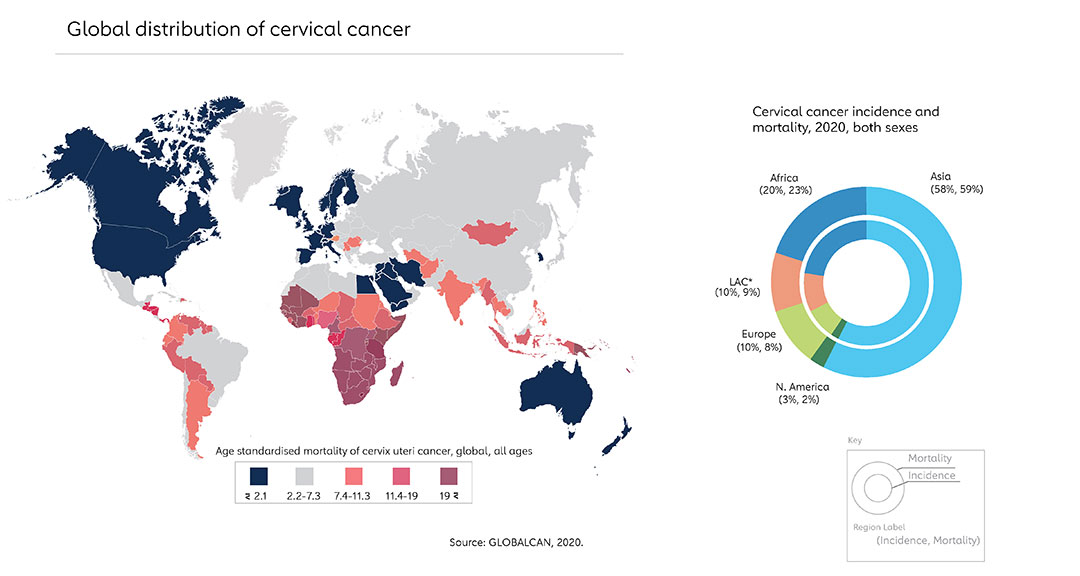
Where does cervical cancer hit hardest?
Cervical cancer is the fourth most prevalent cancer in women, and 90% of cervical cancer deaths occur in low- and lower middle-income countries. The drastic shift in epidemiological distribution over recent decades is due to the availability of effective primary (HPV vaccine) and secondary (cervical cancer screening) prevention tools in most high- and upper-middle-income countries.
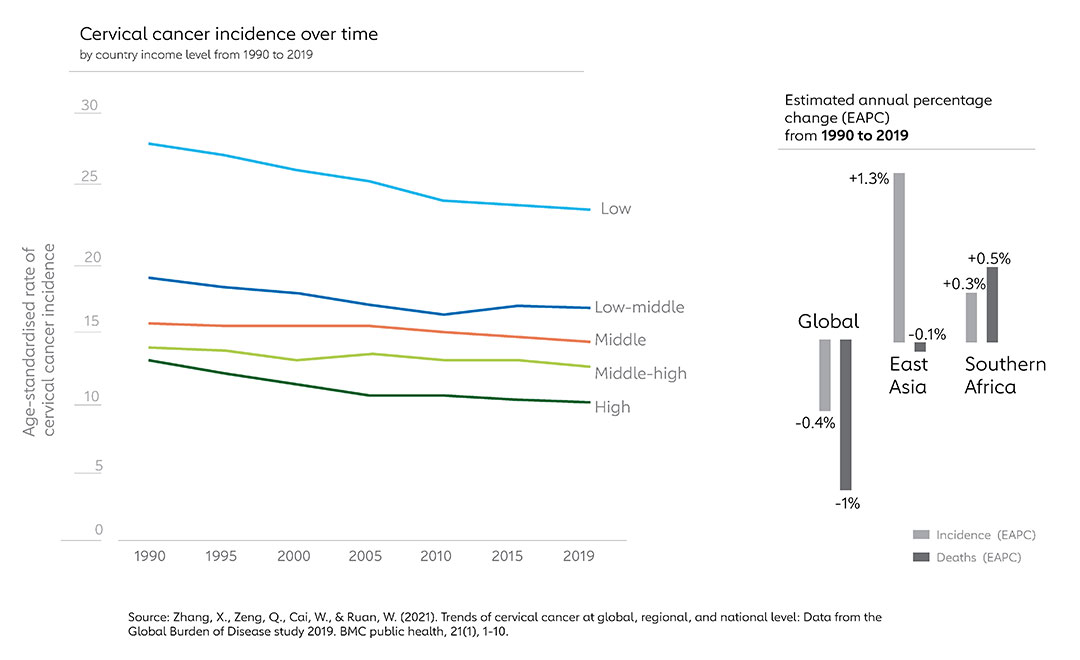
The gradual decline in cervical cancer rates worldwide
Prior to the pandemic, the global trend in cervical cancer incidence and mortality decreased by 0.4% per year between 1990 to 2019, however the equity gap for both prevention and treatment between high- and low-income countries has widened. Regional differences mean East Asia and Southern Africa are the only two regions with increased incidence of cervical cancer in the same period.
Have you read?
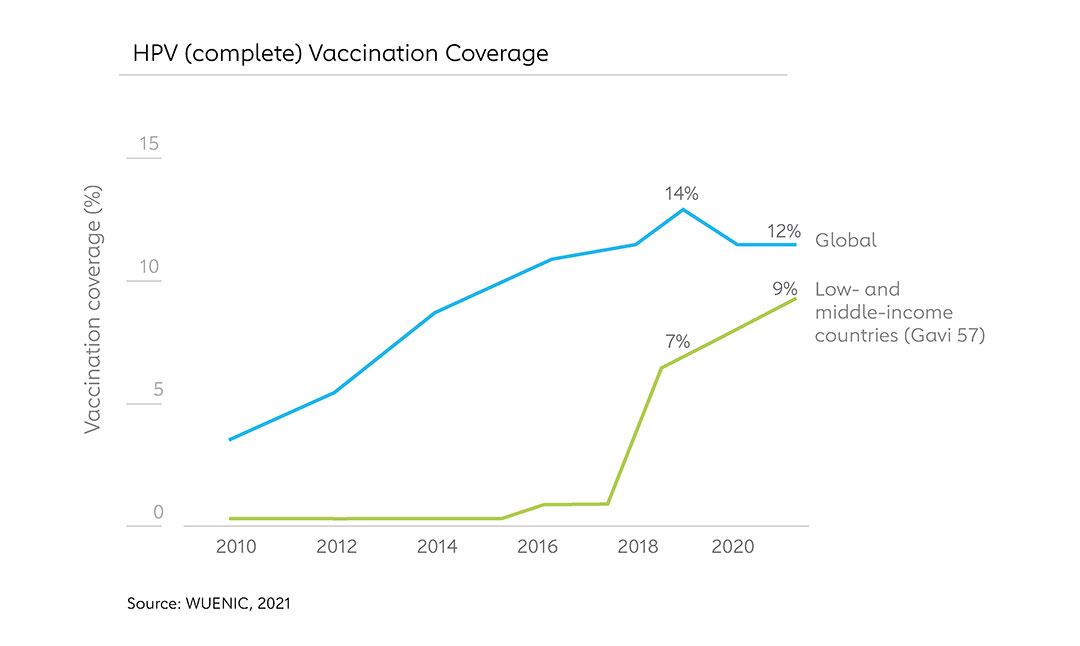
The impact of the pandemic on HPV vaccine coverage
Since the inception of Gavi’s HPV programme in 2012, 27 countries have introduced the HPV vaccine. Thus far in 2022, three more countries have successfully launched their HPV programmes nationally with support from Gavi (Burkina Faso and Lesotho), the most recent in Sierra Leone this week.
But still a staggering 59% of cervical cancer cases occur in countries that have yet to introduce HPV vaccine. This is beginning to change. In total, 19 countries in the sub-Saharan African region have introduced HPV vaccination programmes, and an additional ten are in the planning stages. Some of the most populous countries that share the majority disease burden of cervical cancer in sub-Saharan Africa and Asia, such as Nigeria, India, Pakistan and Bangladesh, are moving forward with introductions in the coming years.
The scale-up of vaccination programmes in Gavi-supported countries means coverage here continued to increase through the pandemic. However severe supply constraints compounded by pandemic-related disruptions led to a stagnation in global HPV vaccine coverage in 2021 (WUENIC).
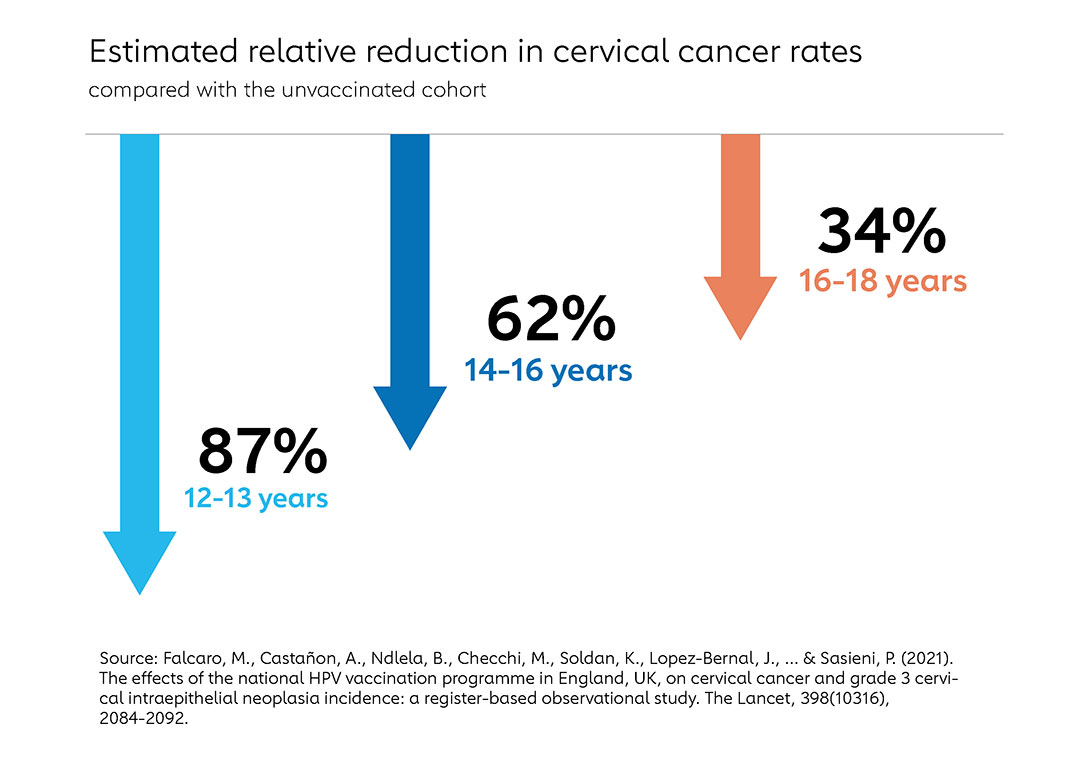
The power of the HPV vaccine
Fifteen years after the first introduction of the HPV vaccine, published evidence on its effectiveness and long-term impact is reaching a critical mass. A study published in 2021 on the impact of the UK’s introduction of HPV into their national programme found that the HPV immunisation programme has successfully almost eliminated cervical cancer in women born since 1 September 1995.
While the evidence for HPV vaccine effectiveness is strong, supply, access and social barriers for demand pose challenges. Alongside the work to expand the introductions of HPV vaccine, advocacy work is critical to address the stigma around HPV, as well as integrated approaches with adolescent health and comprehensive reproductive health services.