Filling the vaccine gap in Kenya
A well-planned immunisation programme can go a long way to reducing the burden of disease on a country.
- 25 May 2021
- 4 min read
- by Mukami Mungai

Nancy was 32 years old when she gave birth to her first child and, being a first-time mother, she was happy and scared at the same time because of the new responsibilities that motherhood had presented to her. Nancy religiously attended her antenatal clinics where a nurse advised her on what was needed to keep her baby safe and healthy, with an emphasis on vaccinations.
“During my antenatal clinics, the nurse emphasised the benefits of my baby getting vaccinated,” she says. “After the baby came, I made all the postnatal visits to have my baby vaccinated. The nurse would tick my maternal health booklet to show that my child had been immunised against certain diseases.”
Additional challenges to regular immunisation of children in Kenya include, according to Kipkemei, vaccine unavailability, low income, vaccine hesitancy, unavailability of healthcare workers, missed appointments and poor road infrastructure.
Her son is now nine years old and she has gone through the same inoculation process for her second baby who is one and a half years old. “Except for a few common health problems such as colds, coughs, fevers, and vomiting, I’ve never had any serious health problems with my babies.”
Lucy Kipkemei, a nursing officer in charge of immunisation clinics at Kenya’s largest hospital, Kenyatta National Hospital, says that low levels of education and lack of guidance from health care workers are among the reasons for under-immunised and zero-dose children. “It is common to find mothers coming to the clinic with babies who have missed doses and, upon asking the mothers why, they say they don't have the information.”

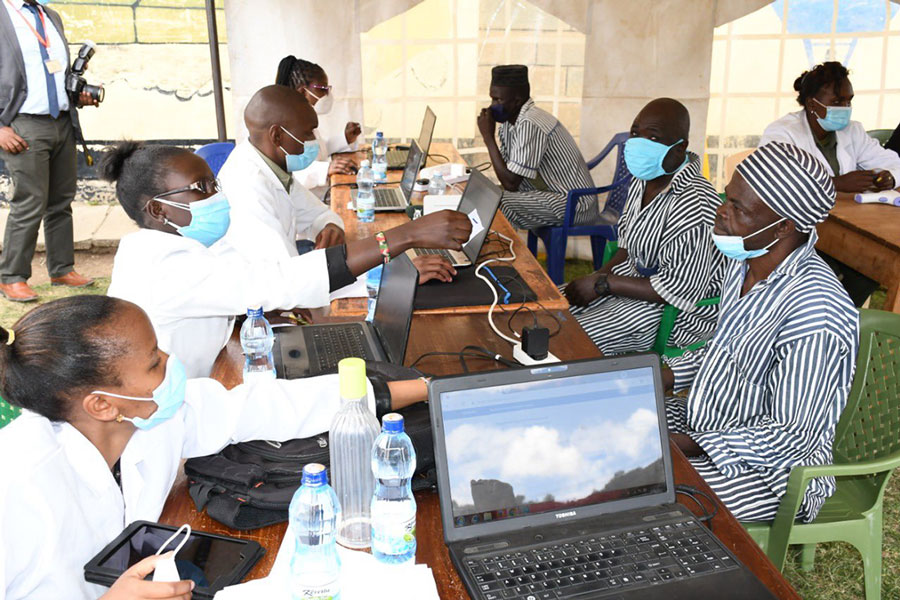
Credit: Mukami Mungai
“Delays in vaccination puts children at risk of certain diseases, including those that have been targeted for eradication,” Kipkemei adds. “Plus it can affect normal growth and other milestones, such as knowledge retention.”
The statutory vaccinations for all babies in Kenya are polio, tuberculosis, pentavalent, measles and rotavirus. These all appear on the maternal health card which helps to keep track of the baby’s vaccines.
Kipkemei explains: “Mothers who give birth in the facility are sensitised during the antenatal period. It is mandatory and it's recorded in their maternal health booklets.”
Additional challenges to regular immunisation of children in Kenya include, according to Kipkemei, vaccine unavailability, low income, vaccine hesitancy, unavailability of healthcare workers, missed appointments and poor road infrastructure.
Jason Kiruja, an Emergency Triage Assessment and Treatment Training Manager at Kenya Pediatric Research Consortium, echoes Kipkemei’s sentiments that vaccine hesitancy and low uptake are driven by a lack of guidance from public and healthcare workers.
Have you read?
“When I got into practice, I thought I knew everything about vaccines, but there is so much that I have learnt,” Jason says. “Planning immunisation services at district and health facility levels, conducting effective vaccination services, strengthening human and institutional resources, suitable financing and increasing access to immunisation services goes a long way to addressing the challenges in achieving fair and equitable immunisation coverage.”
This work is making a difference. According to the WHO/UNICEF Estimates of National Immunisation Coverage (WUENIC), the proportion of children receiving all three doses of basic diphtheria, tetanus and pertussis-containing vaccines (DTP3) has risen from 82% in 2000 to 92% in 2019.
The Ministry of Health has shown commitment to improve and intensify child immunisation services in the country by re-training, empowering and increasing the capacity of healthcare workers and equipping health facilities with refrigeration equipment.
The Ministry, in partnership with Kenya's Paediatric Association and with support from the American Academy of Paediatrics, have designed an integrated immunisation curriculum to guide vaccination training content and structure for pre-service and in-service training for healthcare workers. This curriculum provides information on the history of vaccination; vaccinations for preventable diseases; administration of vaccines; vaccine supply and safety; disease surveillance; outbreak management and data management. This curriculum also ensures the harmonisation of training content across the country.
Kenya has recorded more than a 50 percent reduction in the under-five mortality rate since 2000, from 1,869 to 831 deaths per 100,000 children. Immunisation has made a huge contribution to this progress and immunisation staff across the country are now working hard to ensure it continues.