COVID-19 could become endemic – here is what existing endemic diseases look like
COVID-19 becoming endemic is harder to define than you may think. Here we outline how to know when the virus becomes endemic and outline what existing endemic diseases such as malaria and TB look like.
- 18 February 2022
- 4 min read
- by Priya Joi

COVID-19 is widely being predicted to become endemic. But what does that mean? After two years of living through the pandemic, many of us are hoping we have already entered the ‘endemic’ stage, pointing to the milder cases associated with Omicron. But what does endemic really mean, and is this really something we should be aiming for?
We may well be facing the virus becoming endemic, but we still have control over our choices to invest in reducing this burden as much as possible.
From pandemic to endemic
The shift from pandemic to endemic is hard to define. The terms ‘epidemic’ and ‘endemic’, coined by Hippocrates thousands of years ago, don’t have strict definitions but in epidemiological terms an endemic infection is one in which overall rates stay more or less the same, without huge spikes or falls. The key here is that overall rates on average do not get out of control, so that the ‘basic reproduction number’ or R0, where the number of individuals an infected individual would infect, stays below one.
This may sound easy to put into practice – after all, common colds and influenza are two of the most frequently cited endemic diseases, and these are often thought to be mere annoyances. But diseases such as malaria and HIV/AIDs are also considered endemic despite their widespread occurrence and significant risk of death.
In 2020, malaria killed over 600,000 people and HIV/AIDS around 680,000. That year TB took more lives than both of them put together, with an estimated 1.5 million deaths. Even flu kills upwards of 650,000 people worldwide.
Have you read?
These deaths are tragic, but even when people survive these diseases they face significant consequences in catastrophic healthcare costs, loss of earnings or disability. According to the CDC, the direct cost from malaria through treatment or illness is believed to be at least US $12 billion per year, mostly concentrated in Africa. The cost in lost economic growth is many times more than that.
This is where the definition of endemic becomes more subjective: While these diseases may be controlled to an extent that outbreaks can be managed – is this level of death, health costs, and disability “acceptable”? While there is no easy benchmark we can apply, as a society we must decide how to we wish to reduce these deaths, and what measures we can take.
With COVID-19, what might be useful to focus on is how we shift the response from the intense focus of the past two years to a situation characterised more by prevention and management of acute spikes of transmission. Thus, large-scale restrictions are unlikely to continue for long or to happen again, but ongoing surveillance of cases and other preventive measures, just as happens for flu, will need to happen.
Eliminating further down the road
Just as with diseases like malaria, endemic COVID-19 will probably affect low and middle income countries the most, as wealthier countries will likely have access to new vaccines and booster doses that can keep their immunity topped up, plus good nutrition and access to healthcare.
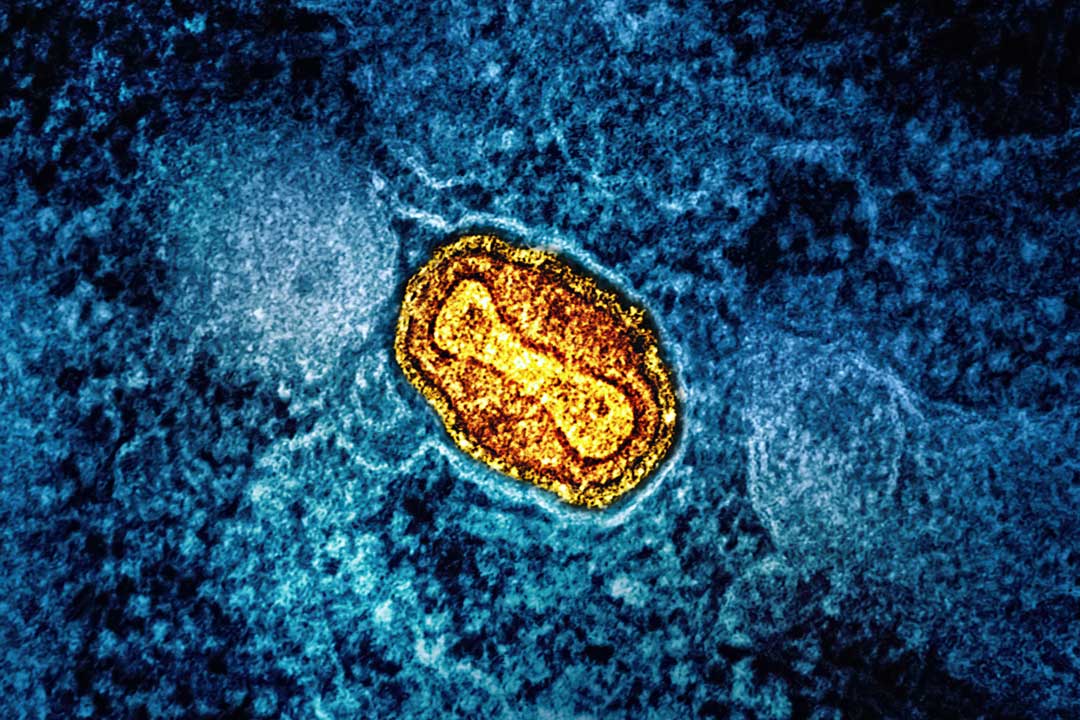
But the herculean task of eliminating an endemic disease may mean the world is never free of it. The only endemic disease to have been eliminated through public health efforts was smallpox. Polio could be next, but only because of extraordinary global commitment.
Billions of dollars have been spent on efforts to eliminate diseases such as malaria and TB, but once a disease is entrenched, it can be near impossible to get rid of. Even with vaccines against diseases such as meningitis, a combination of low funding, inadequate political will and unstable infrastructure and delivery systems has combined to mean that the vaccine does not get to every child who needs it.
The world had the chance to stop COVID-19 in its tracks through a combination of vaccines, quality medical treatment, and restrictions to curb its spread. Now, we may well be facing the virus becoming endemic, but we still have control over our choices to invest in reducing this burden as much as possible.