Can you be infected with COVID-19 without ever testing positive?
Most people who are infected with coronavirus develop symptoms, but not everyone does. So, what assumptions can you make about your level of immunity if you stay well when everyone around you has COVID-19?
- 18 February 2022
- 6 min read
- by Linda Geddes

Your partner has COVID-19, your kids are infected, everyone at work is testing positive for the virus – and yet you remain mercifully COVID-free. Those lucky enough to find themselves in this predicament may be wondering: does this mean they're immune? And, if they weren’t already, does their current exposure to the virus mean they will be soon?
Subclinical infections
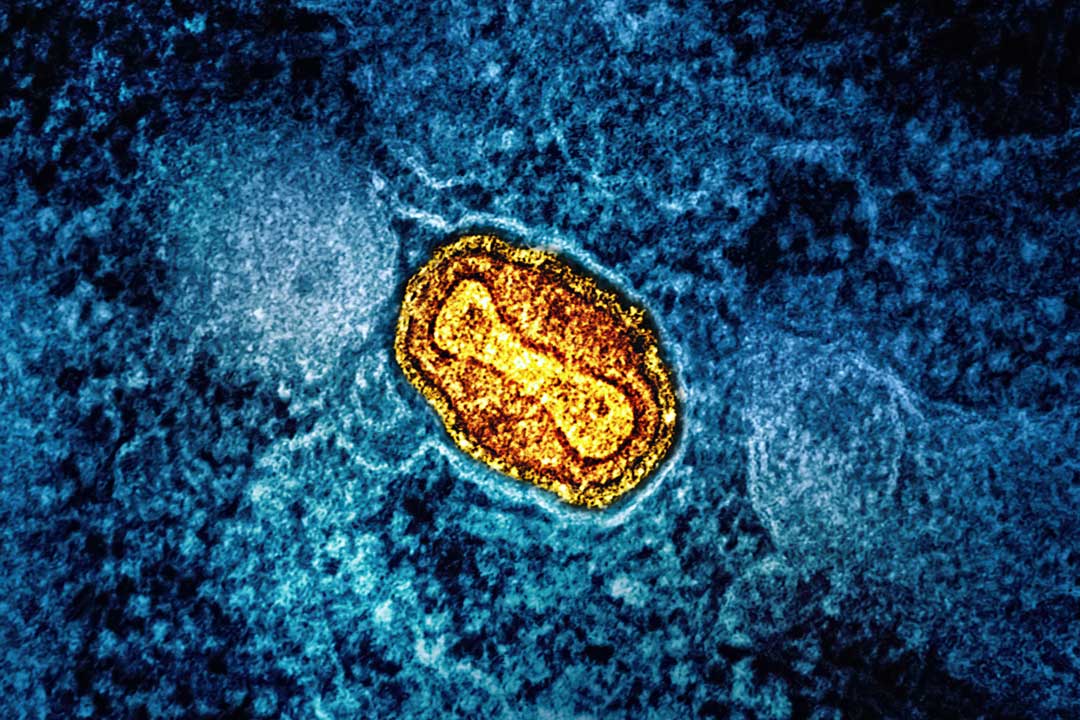
It is possible to become infected with SARS-CoV-2, and shake off the virus without ever developing symptoms. Precise estimates of such “subclinical” infections are hard to come by – if you don’t develop symptoms, you’re less likely to seek a test – but according to one recent meta-analysis, up to 40% of confirmed COVID-19 infections may be asymptomatic. Other studies have suggested that the amount of virus in their airways (their viral load) may be comparable to that of symptomatic patients, meaning they’re capable of transmitting that infection to other people. Indeed, COVID-19 would have been a lot easier to contain if all infected people developed symptoms.
The bottom line is that it’s impossible to know for sure if you’ve been exposed to the Omicron variant, unless you’ve recently tested positive for COVID-19, and you live in a country where it now accounts for virtually all COVID infections.
Some individuals may also become transiently infected, but virus levels in their nose and throat never climb high enough to be detected using a rapid antigen test, such as a lateral flow test (LFT), or even a more sensitive PCR test.
Transient positivity
Researchers at Imperial College London recently published the results of the world’s first COVID-19 challenge trial, which involved exposing 34 young and healthy volunteers to a dose of SARS-CoV-2, and then closely monitoring them over the following days to see who became infected, and how their symptoms developed.
Sixteen of these individuals didn’t develop an infection – defined as testing positive on at least two consecutive PCR tests, which were performed twice a day. However, half of these participants transiently tested positive for low levels of the virus – often several days after the initial virus inoculation – which could have represented the virus gaining an initial foothold in the body, but the immune system rapidly managing to clear it (an abortive infection).
Prof Christopher Chiu, an infectious diseases physician and immunologist at Imperial, who led the study, said: “In our previous studies with other viruses, we have seen early immune responses in the nose that are associated with resisting infection. Together, these findings imply that there is a struggle between the virus and host, which in our ‘uninfected’ participants results in prevention of infection taking off.
“This is likely to be due to a combination of factors, including genetic differences and the speed and size of the immune response at the site of infection, which we are currently studying in more detail.”
Mild symptoms
Some of these participants also reported some very mild symptoms in the days after exposure, such as a stuffy nose, sore throat, tiredness, or headache. These are more difficult to interpret, said Chiu, because such symptoms commonly occur in normal life, and may be unrelated to the infection.
“All participants were quarantined in bedrooms with air conditioning and relatively high air flow, unable to go about all their normal activities, so some mild symptoms may simply have been due to the change in environment,” he said.
“There was no evidence, even in those who had those presumed abortive infections that virus replication had reached sufficient levels to trigger the production of antibodies or T cells or the inflammatory factors found in the blood that are usually associated with symptoms.
Have you read?
“However, some symptoms may well have been related to immune responses in the nose. I think the symptoms in these participants will have had a mix of causes, including the immune system fighting the infection off, but also environmental and subjective factors.”
In other words, even if you develop transient mild symptoms following exposure to an infected person, you cannot assume that you’ve successfully fought off the virus – even though it’s possible that you have. If you haven’t tested positive for SARS-CoV-2, those symptoms could have been caused by something else.
Infection vs. immunity
Neither can you assume that you’re now immune to the virus if you’ve been in close contact with someone who has it. Two different branches of the immune system are involved in responding to infections: The innate immune response is the first line of defence, and, in some individuals may be enough to prevent the virus from gaining a strong foothold in the body, allowing it to spread.
Important as this response is, its components have no way of remembering which infectious agents they have encountered in the past, meaning if you are exposed to Omicron (or any future SARS-CoV-2 variant), the immune system will have to mount an entirely new response, unless you have been vaccinated.
If the virus breaks though these innate immune defences, the cells of adaptive immune response launch into action – meaning antibody-producing B cells and virus-killing T cells. Adaptive immune cells do remember viruses they’ve been exposed to in the past, and this is also the branch of the immune system targeted by COVID-19 vaccines.
If you test positive for COVID-19, virus levels are likely to have climbed high enough that you will mount an adaptive immune response. Studies have suggested that people infected with SARS-CoV-2 develop antibodies irrespective of whether they are symptomatic or asymptomatic – although these do decline over time. The extent to which T cells triggered by asymptomatic infections persist is still unclear.
Safe behaviour
The bottom line is that it’s impossible to know for sure if you’ve been exposed to the Omicron variant, unless you’ve recently tested positive for COVID-19, and you live in a country where it now accounts for virtually all COVID infections. Your best, and safest, defence against future infection is to take up the offer of vaccination when it is offered to you.
If you’ve recently been in close contact with someone who has tested positive for COVID-19, you should behave cautiously around other people, even if you’ve been vaccinated. This means avoiding contact with vulnerable people, and wearing a mask in public places – if your country’s rules allow you to leave the house at all.
It is still unclear why some people continue to test negative while everyone around them is testing positive. It could be that they’ve developed some immunity, but they could also just have been lucky. COVID-19 is still a dangerous disease, so it is also important to continue to take measures to protect yourself.